Neurosurgeon Benjamin I. Rapoport, MD, PhD, presents initial results from a new project exploring the use of embolization to treat brain tumors, particularly meningiomas. Dr. Rapoport covers what happens when a meningioma is embolized, what determines the efficacy of tumor embolization, the experience so far at Mount Sinai, and implications for other minimally invasive surgical approaches to treat brain tumors.
Chapters (Click to go to chapter start) Introduction to meningioma embolization How meningioma embolization works and whether or not it’s safe Efficacy of embolization to treat meningiomas An analysis of Mount Sinai’s experience with meningioma embolization Computation and quantification Goals for identifying tumors for embolization based on location and vascular patterns Implications for minimally invasive surgery Ongoing and future work, and Q&A/discussion
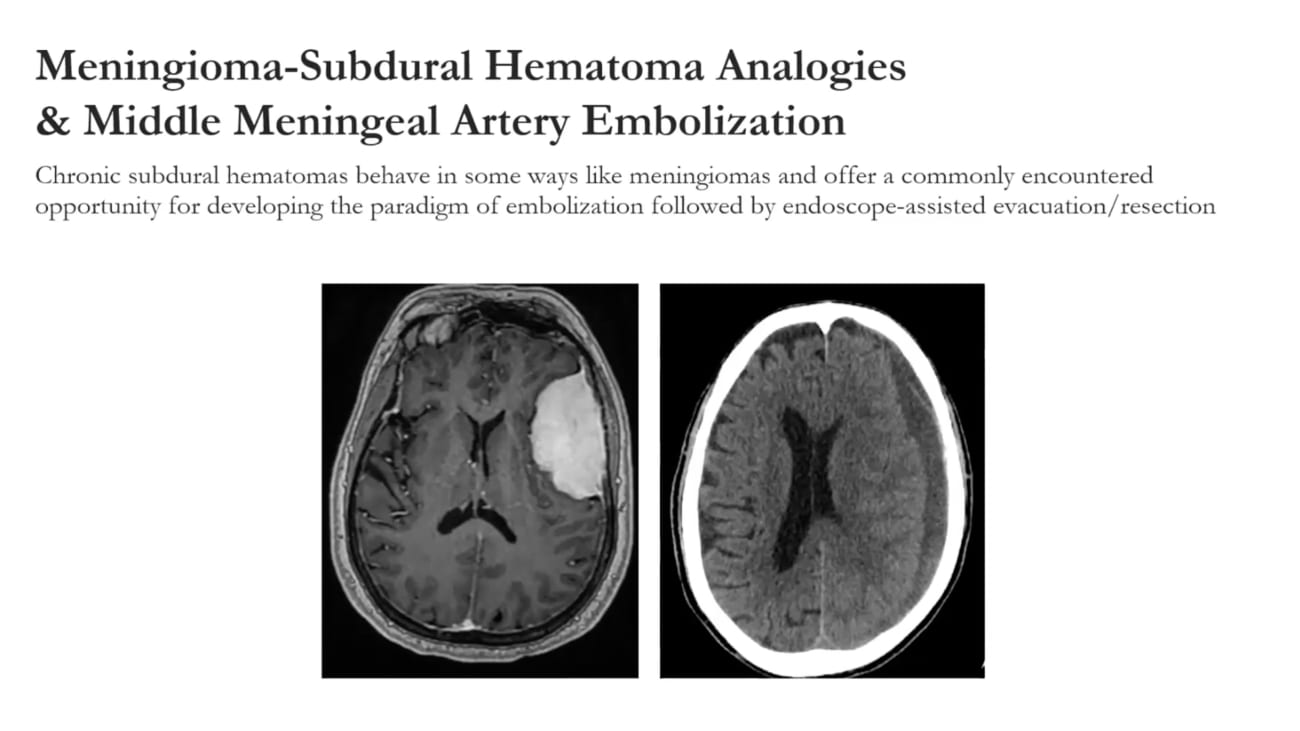
So next up we have dr Ben Rappaport and and I were have known each other a long time. We were residents together. He completed his undergraduate degree at Harvard followed by a masters at Oxford and a PhD at MIT and then his M. D. At Harvard Medical School. He then went on to came back to new york where he is from to complete his residency training at Cornell, followed by including unfolded fellowships in endovascular surgery and endoscopic skull base surgery. Dr Rappaport focuses his clinical attention on brain tumors, skull based pathology and minimally invasive neurosurgery. And he is the scientific director of not signing bio design, leading a team of postdocs and phds who are developing ideas from clinicians among other things into into commercially viable products among other interesting academic endeavors that he can I can tell you more about. Um He has offered a number of peer reviewed scientific publications and has has 10 10 Patents, possibly more by the publication of this slide. Um And he's gonna give us an an interesting talk today. Thanks peter and thanks so much for having me uh my slides up on the screen here. Are you seeing seeing my slides properly? Yes. Great. Is my audio is my audio. Okay, yep. Perfect. Yes and thank you for asking. All right, great, well thank you so much for having me this morning. Um I'm going to speak about a project that we've been working on collaboratively in the department for about a year now on tumor embolization in particular and Ben Ngoma embolization specifically. This is really a collaborative work in progress and I'd like to uh spend some time this morning sharing some initial results and um and really asking for feedback and an insight from from the group and um and maybe for for those who aren't familiar with the work, I hope to to begin to change your mind a little bit potentially about to criminalization. Uh no financial disclosures, but um as Peter mentioned some of the work that I will be discussing this morning um is taking place within bio design. So I do hope that there will be um translational and commercial potential related to some of what we'll discuss this morning. I just want to begin by thanking um huge number of people who have been involved in the work that we'll be discussing because this has really been a very collaborative effort. Um The study involves um both the cerebrovascular group, basically everyone on the on the left hand column has has treated and enrolled patients in this work. Everyone in the middle column has operated on patients um that will be discussed today and and everyone on the right hand column that includes um uh both research fellows and residents and PhD students in bio design contributed to data analysis um and ongoing work. So it's a great, very interesting collaboration, very fruitful and I want to thank everyone who's been involved for the last year. I'm going to begin with a personal anecdote um just to share really how I got interested in this subject of meningioma mobilization. And um I think this anecdote in some ways encapsulates a number of the key issues as I see them in into marginalization. So this um this these images are images that I saved in my iphone for the past five years. And that's the case that I was involved in as a resident. It was an elderly woman who had a a large convexity extending to the subpoenaed wing meningioma. And uh and she was referred for preoperative embolization and where I trained at Cornell. That practice was as it is in many places um where preoperative embolization is done. Uh two usually to symbolize the tumor. Um the day before surgery and the workflow, which I think is the most common workflow at least in the United States is for the patient to to arrive at the hospital on the day of embolization to be admitted for embolization and then admitted post globalization and go straight to search for usually the next day. And uh and as a result um the patient has usually there their preoperative M. R. I. Is done on an outpatient basis and they don't have another M. R. I. Until uh the post operative period. So there's never usually a chance to see what happens on some level uh after embolization. This patient. Um Just for logistical reasons. The the surgery wasn't, the amputation was done on a thursday. And and the surgery was done on a monday. And so the patient was in the hospital over the weekend and her preoperative planning MRI was done um the month monday morning, the day before sir, the day of surgery. And um and so what I'm showing here on the left is the the out patient preoperative M. R. I. On the left here um showing an avidly contrast enhancing tumor. And and the right hand panel is is still a preoperative M. R. I. Preoperative contrast enhanced MRI. Um And but it was done after the tumor embolization two days after the tumor embolization. And obviously what you see is that the the tumor which was extensively analyzed. Um I don't have the I don't have the anti graphic images but don't worry. There are plenty of those coming later in the talk extensive embolization and an almost complete loss of contrast enhancement in the and at surgery this tumor was completely ah liquid if active necrosis basically. Um totally aspirational, very straightforward reception. Which was fortunate for you know an elderly patient who could have had a obviously a complicated complicated operative course. So this this episode kind of sparkly interest in the whole subject of what what happens with globalization because um I think many people think and certainly the literature reflects that embolization, preoperative lee is all about blood loss. It's all about preventing operative blood loss. But this case um really sent me to asking the question of is there something else besides limiting blood loss um that tumor verbalization does to the tumor in the preoperative period. And are there other ways we should be thinking about um why to perform mineralization and how to assess the efficacy of globalization? So with that as a kind of prelude, I'll jump right into what we've been, what we've been doing. Uh So I'm gonna talk first a little bit about um technically how manageable embolization works. Uh And I'll show just a little bit of the evidence on whether or not it works. And there's certainly disagreement on that subject. Um And then I'll talk about the work that we've been doing over the last year, uh starting with what seems to happen and geographically radiographic lee otherwise, when a meningioma is symbolized, and then we'll talk about how do we assess the advocacy of globalization? And that's not a straightforward question. And then I'll talk a little bit about our experience uh here over the last year, and maybe even a little bit before that. And we'll talk about ways that we've been approaching quantitative in of understanding the efficacy of tumor embolization and angio embolization in particular. And this is work done by one of the PhD students who is working with us in bio design and engineer from Rensselaer polytech Denzel Faulkner and and then we'll talk a little bit about future work and where we hope this is going um And and I hope that we'll get also to questions about whether it makes sense to think of alternative ways of approaching these tumors once they are emphasized. So how does an angio embolization work? Um Many people are familiar with the process. So just as an overview um a patient undergoes a catheter angiogram. Um And that's what is shown here here. You have a patient with a large screen old wingman ngoma uh in the left hand panel um and in the preoperative period uh usually a day or more before surgery, the patient undergoes the diagnostic angiogram. Um And and hear what you see in the middle panel is um an external carotid injection which in the ap and lateral um projections shows you uh the vascular blush of the of this keynote indian ngoma. And um after fully characterizing the vasculature of the uh the brain and the tumor. Um the the feeding of arteries are selectively micro pasteurized um and and through a micro catheter. Um Any of a variety of normalization agents can be can be used to analyze the tumor and those include glue and onyx particles. Um And there are other options as well and we won't get too much into the um into the specifics of the implications. I think I'll result preserve that for another another talk. Uh There's a ton of interesting engineering going into that right now. But we'll reserve that. And so here what you can see is that the the tumor which has a very avid vascular blush has been at least from an geographic standpoint, completely de vascular arised in the right hand panel here on the post stabilization, uh angiogram. And we we say that that shows a a loss of tumor blush. So well this has been done for decades. Um and what do we know about whether it works and what we know about whether to memorization works uh really depends on how we define works. And to date over the last really two decades, the goal of preoperative meningioma globalization has been to reduce inter operative blood loss. And I'll just say this is a very controversial topic. And uh there are a number of meta analyses out there for which I've just put on the screen here and they are conflicting. Some of them suggest that um that there is no difference in inter operative blood loss from uh embellishment and dioramas and and some suggest that there is a benefit in terms of blood loss reduction of blood loss reduction operative time. Um when a minute, one minute, you always are analyzed, of course there's a tremendous bias in which tumors are sent for preoperative embolization in the first place. Um And I would also point out and the residents have probably heard me say this number of times that the whole idea of trying to quantify operative blood loss is pretty difficult. And and as we all know, um estimated blood loss in a neurosurgical case at least. And probably in most cases it's not really a particularly good measure of actual blood loss. Sometimes it's almost a random number. So when um when these cases are retrospectively reviewed and uh and love loss is taken as an indicator of efficacy, one has to do that with a certain degree of suspicion. So one Wonders, you know, is there something else that we can measure? And and it is blood loss even the whole point at all? And uh and of course, you know, total blood loss in the case um is not just tumor related blood loss, there's also blood loss from the exposure. So there's all kinds of issues um to wonder about in how the efficacy of an NGO memorization has been interpreted in the literature today. So I think that we'll have something to say about about that through the Montana experience over the last year and beyond. Well what happens to a tumor um after embolization, let's talk about what happens and geographically, we sort of showed that in the last in the last uh slide um the uh from an and geographic standpoint, the the the procedural ist tries to d vascular rise the observed tumor blush. And this is exactly what I was showing in the previous lines. But what happens on M. R. I. And as I mentioned in most institutions, it's not common to obtain an M. R. I. After uh normalization of the tumor. That would be a third M. R. I. Scan. Usually. Usually patients obtain preoperative, which would be a preoperative preamble Ization M. R. I. And a postoperative M. R. I. Which would be a post operative and post and post embolization M. R. I. Um But of course that leaves no way for M. R. I. Imaging to um to assess the effect of globalization alone. And um what we've been doing over the last year here is to obtain a third M. R. I. We have a study protocol that we've put in place um that we put in place last year that involves obtaining an M. R. I. After embolization and before surgery. And that has given us a real window uh into understanding something about what happens to these tumors after after their ambulance. And this is um this is an example of that. And so in the top left, you see the axle post contrast preoperative preamble ization uh M. R. I. Um And in the bottom you see the corresponding diffusion weighted uh sequence. And um in the top right. Um And on the bottom right, you see respectively the Mhm. Post embolization preoperative contrast enhanced Tamara. And what you can see is that after embolization, there is almost complete loss of contrast in the tumor. If you if you don't look carefully, you can almost think that um that there's been a tumorous section but there hasn't. And uh in the bottom here you see uh some diffusion changes as well reflecting maybe early tumor necrosis. And not in all cases. But in many cases there is a major change in that texture and firmness of these tumors which really facilitates uh humorous section. And I'll show you some examples of that. Here's another case. Um This is a parasite vaginal meningioma that we that we emphasize pre operatively. So here are the here are the preoperative preamble. Ization, Axial satchel criminal uh sequences. And here are the corresponding some of the corresponding images from the angiogram. These are just micro catheter injections. So on the left hand panels you see the you see some some ap projections of micro catheter. Selected me mike some micro catheter injections. This one on top is showing you an injection through the middle managerial artery. And you can see um in the late arterial, early early capillary phase you can see the tumor um capillary bed being filled with contrast. And you can see a similar sort of picture uh in the lateral projection here on top. Um And in the right hand pains. You see this is this is actually taken during uh during um injection of onyx into the tumor. And uh and you can see uh the liquid embolization really penetrating into and filling the tumor. And finally here in the bottom left, you can see that we've we've injected liquid anabolic agents from from both both middle managerial arteries. One of them crosses the midline to fill part of the tumor. Um And you can see this cast of the anabolic agent filling filling the tumor and the um and some parts of the mental energy artery. And and we've as I'll say a little bit later on some of these some of this vascular anatomy is becoming increasingly familiar to the group because um there's just so much, so much experience now um here and across the country uh emphasizing middle energy artery pathology in the context of subdural hematoma. And I think actually there's some very interesting overlap in these pathologies which I'll discuss a little bit later on. So here um here again on top is the preoperative MRI. Preoperative preamble ization MRI. And on the bottom we have the still preoperative but post embolization M. R. I corresponding sequences axial sagittal and corona. And again, what you see here um is uh extensive loss of contrast enhancement in the and um Now what does that actually mean from the surgeon's standpoint. So, I want to give you um a sense of that. So these are some images taken from the case. Um So I'll show you a video in a second. Um But here the the tumor um here you're seeing the tumor capsule has just been incised and the tumor is basically completely Almost 100% the vascular honest. And it has this sort of marshmallow fluff appearance to it, which makes it completely aspirational and very easily handled that surgery. And let me see if I can play this video just giving a sense of how this handles after embolization. Um so again, the capital has been in size. The tumor is basically being split in half and you can see there's almost basically complete the evacuation of the tumor that's over there is the onyx cast of the of the implications. And um and the team are in this case is basically completely as for Abel from the inside. Uh here here's a piece of the tumor and gross gross pathology. So um That is all by way of sort of motivation, motivation. And and now I want to ask the question of, well again, what what determines the efficacy of embolization both. How do we measure how effective the mobilization is and what are we trying to achieve in the first place? Because you know, 20 years of looking at this problem have really defined embolization efficacy as in terms of inter operative blood loss. But I'd like to ask the question of, can we define a concept of globalization efficacy beyond simply inter operative blood loss. Knowing that or at least thinking that globalization has some impact on these tumors beyond just revascularization to somehow improve the ability to handle the tumors intra operative I guess as I was just trying to show in some of these cases. And another interesting question and really an important one to ask is what is an important control And and this comes up all the time. People say, you know, well how do you know that uh the tumor wasn't already wasn't already a marshmallow fluff before um realized it. How do you know that the embolization is responsible for changing the consistency of the tumor? Um You know, you you only have one shot to operate on it so you can only open that open the head once in these cases. So how do you know that what you did had had any impact? And that's that's a challenging question to answer. But I think I do think that these additional M. R. I. Sequences um post embolization, pre surgical are gonna shed some light on that subject. And there are a number of additional variables that that come into play. And those include tumor location. That's where anatomy of the tumor tumor biology because we're actually symbolizing tumors that are not just energy almost. But today we're focusing specifically on them energy aromas and even even within meningioma is there's a fair amount of heterogeneity as as as you know. Um And then of course there's differences in the symbolic material so we can use particles glue, onyx or coils in some cases, other things. And then of course there are differences from from surgeon surgeon and immobilization technique and um there are differences in the timing of embolization relative to surgery. So as I mentioned before in many institutions, the most common practice is to analyze uh the day, the day before or sometimes even the day of surgery. Whereas in europe for example, it's more common to wait several days between globalization and surgery. And um there and there's a thinking around that, that perhaps um if there is some early process that is happening after embolization, does it even make sense? Perhaps intentionally to leave a couple of days between embolization and surgery? So all of these variables are potentially important. And um how do we go about uh weighing their relative contributions in a systematic manner? Um so I'm going to focus really the current discussion primarily on the an atomic variables. And uh and we'll save some of the other variables for uh for future conversations. Um And in the next few slides, I want to give some intuition around uh around the thinking on an atomic variables that have the most impact potentially on what will come to define as the efficacy of of meningioma globalization. So here's another case. Um a convexity. Meningioma not too different from the parasitical one that I showed a few slides a few slides ago. Here's the here's the preoperative preamble Ization mm Our study and here are some uh some views from from this patients uh embolization angiogram and what I want to highlight here um is uh both the the different contributions different vascular beds contributing to to this tumor. Um So on the top left, you can see that the tumor is is substantially fed from the branches of the external carotid artery in particular for middlemen in the lottery. Um And we did in fact both middle energy lotteries, both the left and the right contributed to this uh this tumor. Um But also you can see this in particular after the embolization has been performed. Um There is a contribution to the tumor especially to the sort of feel surface of the tumor um from internal carotid artery branches. And uh and I didn't say this explicitly but we we really seek not to symbolize through into the internal carotid artery branches most of the time. Certainly not. Um M. C. A. Or a. C. Distal branches. And and what I want to highlight here is that in many cases what limits the extent or the efficacy of cannibalization of these tumors is the degree to which they are vascular. Rised by the internal or external karate branches. So here what you're seeing in this image with the arrow is after the tumor has been emphasized through the bilateral minimum geul arteries. There is a residual feeling of the uh of the kind of um inferior aspect of the tumor from uh distal branches in particular of the middle cerebral artery. Also from the anterior cerebral artery distal branches. And you'll see that the this tumor was at least on our post embolization. M our assessment. I was not completely mm belies. Although you know of course we don't know totally what this means. But now we're looking at the contrast enhancement pattern following embolization. And you can see that there has been loss of contrast enhancement in the more superficial aspect of the tumor. Um But the the deeper aspect of the tumor uh the inferior aspect of the tumor um retains its contrast enhancement. And that corresponds to this part of the tumor that you can clearly see uh still has its vascular blush after the external provided feeders were taken. So I'm trying to kind of compile a compelling body of circumstantial evidence to try to convince those of you who are skeptical. Um That that there's a clear relationship between what we see and geographically and what we see on on M. R. And this is not this is not this is this is not typically how tumor embolization has been evaluated. So I'm trying deliberately to make as compelling a case as I can. Um Here's another case. This is an orbital roof. Meningioma and I'm not going to show quite as many images but again similar idea here. Okay, so um on the left uh axial sagittal coronal views uh preoperative preamble ization of this relatively large uh large and contrast and added the contrast enhancing. Been ngoma and in this panel here the second from the left, you can see the post analyzation preoperative M. R. I. And again you can see that a chunk has been taken out of the contrast enhancement pattern after embolization. But there is still a lot of contrast enhancement. And what why is that? Why were we not able to symbolize? Why were we not able to reduce the total contrast enhancement to near 0? And the answer is that this patient had this tumor was fed both by the middlemen and deal artery. Uh And as is often the case in the no spin or doing an NGO Mazz and his orbital roof meningioma is by branches of the epidemic. Are and and because because of the high risk or at least the greater risk trying to amb allies through the ophthalmic then through external collided branches we did not and typically do not uh symbolize through the epidemic. And so whatever whatever portions of the tumor are still being fed by by the ophthalmic artery are still basically appearing to contrast to to enhance with contrast in the post embolization M. R. And there's a certain amount of um let's call a hand wavy nous to the to the explanations here. I'm trying to tell a story and not all of the I'm trying to convince you without all of the rigorous data yet required uh to to do so. But I want to at least give you some intuition into where the hypotheses for some of the studies are coming from. So um all of that in its sense is really just uh intuition and motivation and and now we want to try to see what we can do to make some of it rigorous. Um I hope I've at least uh convinced some of the skeptics that there's more to meningioma mobilization than just limiting blood loss alone. And that there may be some utility to looking at the contrast enhancement pattern on the post embolization preoperative M. R. I. As a way of understanding what's happening to the tumor on some level. Um And so we have put together a study protocol that allows us both to do both retrospective and prospective analysis of their radiographic imaging both and geographic and NMR And and also to allow us in a prospective manner to um to obtain additional M. R. Sequence in the post normalization preoperative period for these patients we have um in the 2016 to 2022 period um here at Mount Sinai symbolized almost 100 meningioma as and all of those who are in the process of evaluating in a quantitative fashion. Um Where there is additional M. R. S. We have been doing it in a quantitative fashion and where there is just angiography in a kind of semi quantitative fashion. And and to date in the last year we have almost 30 patients in this three M. R. I. Series um and all of those as I'll show you in the next few slides have undergone volumetric quantitative analysis. Um And so what we've tried to develop. Um And and hopefully I've I hope I hope I've justified in at least an intuitive fashion. We've tried to develop this notion of extent of globalization and the term the terminology there is meant to kind of reflect uh the terminology used for extent of reception in in um in tumor surgery. We don't know if it's efficacy of globalization. We just we can say its extent of embolization as defined by the degree of contrast enhancement on the post embolization M. R. I. Just the exact same way that um extent of resection is defined when you're talking about um tumor surgery. And so what we've been doing is um for every case that comes and has that additional um inter mmR study. We have we have been going back and doing a full volumetric analysis uh of of the case and here's how we do it. So um we um we basically take the in the in the initial presenting M. R. I. We uh we compute the volume the volume of the of the tumor before any intervention. And then in the post amortization period. Uh We measure the contrast enhancing volume of the tumor and the non contrast enhancing volume of the tumor before reception. And we define that. Um We've been defining the extent of embolization in just the same way you would define the extent of reception if this had been a respected. Um And so the percent we give it as a percent percent of globalization is the basically the percent of tumor volume that is non contrast enhancing on the post embolization. Um M. R. I. And so I'll show you just a couple of cases. Um but I think you can understand what's going on here. So here in the left hand column is the pre intervention uh case. Here in the middle column is the post intervention, the analyzed tumor that has been segmented. And this, you know, this does require um you know, computer aided analysis because the shape of the contrast enhancement pattern is um is often kind of tricky to handle. It's not something that you can approximate in a kind of a times B times C over two approximation the way we sometimes do for um for mass lesions that is not possible for these tumors. You really need a volumetric, careful volumetric analysis and we're doing that in an increasingly automated fashion. And these um these images in this this part of the quantitative assessment really a student, Denzel Faulkner, that PhD student from Rensselaer polytechnic I mentioned is working with us in bio design And uh so this this particular tumor is one of the first ones I showed you earlier, 91% analyzed. Um This is another one in our in our series. Um you can see it's largely immobilized but still incomplete and by volume We get almost 60% analyzation extent. And um and here is one more just for Just for comparison a medial screen Idol England ngoma. That as we've been learning um had significant uh significant supply also from the anthemic. And for that reason was only 31% emphasized. So where is this where is this taking us? Um Where I hope to be in in in six months or a year. Once we have accrued a number of more patients, we're already seeing distinct patterns in in the ability to empathize to us based on location and the correspondence between tumor location and vascular and vascular patterns. And on some level this is you might say this is obvious. Um It's obvious once you start looking at it, it's not necessarily obvious until you start looking at it. But there are there are clear patterns that emerge um in the vascular supply to the U. S. And the corresponding extent to which they can be completely immobilized. So for example, if you kind of categorize uh you know, um Meningioma is by the classic locations. And here I've just made a cartoon showing some of the classic locations. E for example, is the kind of convexity meningioma that everybody knows and loves. And those uh those convexity Meningioma tend to be almost exclusively supplied by the middle energy artery. If they're more more posterior. Oftentimes there is a uh Oftentimes there is an exhibit of branch also that feeds them and those uh those tumors we're seeing at least in a slightly more than anecdotal uh way now um can typically be very extensively analyzed uh similarly. Um The lateral spinal alignment NGO must see are often almost completely supplied by middlemen and deal artery and uh as there is or or or you know other internal maxillary artery branches and can often be very extensively analyzed. And we're increasingly now due to analysis like this, able to quantify that. And I hope by the time we have, by the time we have 60 or 80 patients in the three M. R. I. Study group will be able to do that in a really quite rigorous way and develop um what I'm trying to call kind of an atlas of tumor embolization here. And you know, we often ask which patients, is it uh is it even useful or justified to do an angiogram pre operatively to see if they can be um if they can be analyzed. And I think some of this work will begin to answer that question. And uh you know, not surprisingly, the tumors, the d tumors, the tumors that are either medial solenoid wing or cli level or client ID all more um more towards the middle cranial fossa, midline. Um Those tend to be much less amenable to mm normalization through external carotid branches. They tend to be fed by um by the single hypocrisy or drunk or by the infra lateral trunk and not easily analyzed at least by liquid or particle uh ambala occasions. So um we are developing an intuition around this now and I hope that um maybe in a year from now, we'll have enough patients accrued to really say these things in a in a rigorous way. Um and now in the last couple of slides I would like to to show um something maybe aspirational uh that that we have tried to do. And we have sort of started thinking about and that I really hope will be one of the outcomes of this uh of this work. And that is that not only will we learn more about the tumor embolization, the biology and physiology of what's going on in these tumors, but well be able to change the surgical approach to these to us From uh from a maximum invasive cranial surgery to something uh in some cases or minimally invasive. So here is a elaborate funeral wingman ngoma. This was a 70 something year old woman and she had already undergone multiple other medical procedures in her in her life. And this is presented as a a surprise to an already complex medical life that she had been living. And ah and fortunately, um fortunately this tumor was extensively extensively and almost completely embolism ble through ultimately through her middle managerial artery. And so you can see now you're used to seeing these collections of images, the post embolization, preoperative m. R. Showed almost complete um loss of contrast uptake i in in this tumor. And so this is this is a patient of dr Pedersen's actually. And in the in the morning conference uh in which this was reviewed, I remember Dr Pedersen said well you know maybe it's maybe it's possible to do a more minimalist approach to this tumor. We don't know what what if the tumor is more liquid active necrosis now than um than solid tumor. And would it be possible to um to attempt removal through, let's call it a large barrel. And it was not as straightforward I think as um as we might have hoped. But I think that the the idea still stands and I do hope that this will be something we um we continue to attempt. And ultimately it did it did it did work out um to to not have to do a full size traditional craniotomy, stereo type craniotomy for removal of this meningioma. And I think that um you can see here the the tumor was it was this fluffy white um color the same way as I showed you that marshmallow tumor at the beginning of the case. Although this was more fibrous and difficult to remove. Not as easily as credible. And we do find that some of them even when completely de vascular arised don't become that they don't develop that soft texture. And we don't totally know why just yet. Um But I think the idea still is that if we can convert some some of these um you know some large craniotomy is into a smaller craniotomy is. And the more minimally invasive procedures there's something to be gained from globalization beyond just limiting blood loss from the approach really to fundamentally changing the way you think about how to approach even some of the very large, at least lateral to united wing and convexity tumors. And I want to maybe go out on a limb here just a little bit. And um I kind of alluded to this earlier, but uh as a group, we've seen it just a tremendous uptick in the number of embolization procedures we've been doing over the last say five years because of the um the interest in chronic subdural hematomas and possibility that middle managers artery embolization represents a um either an adjunct to the treatment of uh chronic subdural hematoma or even potentially a standalone treatment. And while the, I think there is a there is a gathering of momentum around the idea that that's the case. Um Still, the uh the randomized trials are still enrolling so we won't we won't really have uh level one evidence on that for some time. But um, but still we we have more and more experience looking at the angiograms of chronic subdural hematomas and they do look in many ways like convexity meningioma and there is some and some may be understanding or intuition that we can give for why that might be the case. And we now know that uh we now know that basically um you might think any lesion that sits in close opposition to the dura for a period of time recruits some of the same vessels that uh that supply the dura. That may be sort of a hand wavy intuition for why that that is the case. And certainly um that does seem to be on some level what is happening. And so I think that although this type of case that I showed with a convexity, wingman ngoma, maybe more more hard to come by. Um the idea of a embolization followed by a endoscope assisted borehole type procedure to treat a convexity lesion is going to be increasingly common. Uh And so I'd like to show you just one case along these lines. Maybe just as a as a little bit of inspiration. Certainly it's something that has interested me over the last year. This is a patient with a cute on chronic subdural hematoma who did undergo um who did undergo middle managerial artery embolization. And uh now in light of the tumor mobilisations, we've been showing, you can see at least on an intuitive level how sort of similar conceptually the amortization is for humor and for some Julian martoma. And and this uh is an endoscope assisted evacuation of the uh of the hematoma. And this is this is just the endoscope working through a burrow hole. Uh and you can see here um this is the cortical surface. This is the this is the subdermal membrane that we're getting rid of. Um And you can see that even through all these um endoscope assisted procedures give it uh excellent visualization. And there's even a fair amount of instrumentation uh that is um helpful through through the variety of endoscopes that we currently use um in these subdural hematoma cases. Uh You can you can irrigate, you can use the bipolar Kateri through the endoscope as I'm doing here. Uh And and you can um you can also use the uh endoscopic grasping forceps and other instruments to try to remove um both the membranes and pieces of the of the hematoma. Um And this isn't in many ways a much easier case than uh than trying to remove him in a coma through a large bore hole. But I think that the intuition is still there and um and I think that these these cases may give us an opportunity to kind of practice some of the techniques that we developed them um in the kind of conscientious way, maybe increasingly useful in transforming some energy. Um A surgery's into more minimally invasive, more minimally invasive surgeries. Um So I hope to be able to come back, you know in a year or a year and a half and show you a full 100 patient case series on this on this work. And I think when we have that those kinds of numbers will be able to say, some more definitive things, especially about the an atomic patterns and the patterns of revascularization that we can achieve. Um but there is a fair amount of ongoing work uh with this whole collaboration, especially with the group of bio design. We are increasingly automating the image analysis both the volumetric analysis of the tumors on M. R. And uh the and geographic images obtained in the angio suite. We will be compiling this as a very quantitative atlas of a meningioma, vascular anatomy with the classification both by um mm our degree of vascular vascular ization and classified by um by vascular pentagon. And we are working um in work that I hope to present in the future on a very interesting novel anabolic agents and uh with um a small startup company on a novel embolization uh micro catheter. Um so thank thank you very much for giving me the opportunity to present this morning. Um and I'd be very happy to to answer questions and uh and to um to hear your thoughts. Thank you Ben. Fantastic talk if I can make a few comments in general. Um so you know, one of the things which I think is becoming more and more apparent as you know, and you know, I had a recent journal club with the residents about this from a recent nature paper from the Toronto group is that really when we think of meningioma as being these homogeneous tumors. They in fact have a complex heterogeneity and they have a fairly reproducible and also equally complex genomic profile. And I think the more we begin to understand their biology and their specific I would call it fanatic behavior. I think the more this will give us insight into the patterns of embolization, vascular vascular charity and treatment. And I think what we're seeing is not just variation in the genomic profile, but epigenetic changes to based upon the location along the skull base and convexity. And I'm sure there's some other linkage there too which would be, you know, relatable to the not only vascular profile that you're seeing, but the the degree of efficacy as well. So I think combining some of that work as a next level kind of analysis will be really fascinating to see. Um and then the second point I want to make is that I think, you know, like you and I have discussed, I think that there is going to be a lot of MRI based, you know, almost prognostication that we can begin to develop, which is I believe quantifiable And I think there's patterns in the edema. For example, there may be patterns in the diffusion and the T. two signal and I think beginning to think algorithmic li about how these are predictable for not only embolization extend to resection and outcome is really going to be I think part of this whole um you know the way we look at the this category of tumors and to start to think more broadly more complex about this whole surgery uh maybe different than historical ways where we just thought you know meningioma, how do we take it out and elaborate approaches? So really nice work. Ben. I'm really very happy. Thank you for involving me in this project as well. Thanks so much for the for the collaboration. Yeah. Ben, it's a really good analysis. It shows that just like with subdural hematoma, inter cerebral hemorrhage and many of the things that we have long thought of as a dormant type of pathologies by applying new technology and new thought processes. We can make advances that we didn't even think of before. Um One of the things that we've discussed that I didn't see as part of your plan but I would like to see as part is the concept of micro navigation too. The enhancing areas that remain after embolization to add histological intra operative blood loss maybe with a flow meter but to add inter operative analysis of heterogeneous areas after embolization um you said before one of the problems is that you can only operate once. Right? And so you can't operate on one that's not been immobilized and one that's been immobilized but there are areas of humourous that have not been immobilized and we can micro navigate to those. So really with one operation you do get a chance to look at both a nimble ized parts and embellished parts. And you can have it Back analysis of those two histone pathologies or inter operative findings or some sort of inter operative measure. We've discussed whether it would be a flow meter or some maybe even fluorescence, but you do have the opportunity to look at Both parts of the two murders. Um That was one thing and then I I see that J is here J I wanted to ask you about the comment that was made earlier about the two different types of vascular supply because one of the best outcomes I've ever had was the tumor. Um belies where you did kill it through the minutes ago hypothesis ill trunks. This is the one that ray knows about. Um And so even even though it wasn't an M. M. A middleman in jail artery, it was one of those deeper I see a based arteries and I would like to push be able to push that envelope a little bit as well. So I'm interested in your your thoughts about that. You're on mute now jay thanks. Always saying people are so don't be when they do that. But um in any case uh Yeah, I think so. The first of all I just want to start with saying Ben amazing work. Like I remember I was talking about, you know, doing this sort of thing two years ago before you've been hearing the rigor you're bringing to it and the way you're putting it together and the thought, you know as you're presenting your stuff. I'm just thinking of just the way you're going to lay out your papers to help educate the entire community in the world about this and essentially create a body of work and a and a foundation that's gonna allow us to figure all of this out. And that ties exactly the doctor Henderson's question, which is um which my answer is, it's the complexity of what we're trying to do. We talked about Roger said meningioma or heterogeneous. Exactly. We're talking about symbolizing meningioma as we're talking about a disease where some are rock hard calcium somewhere super fibrous, some are completely soluble. They're clearly completely different lesions. Right? And then we're talking about embolization like it's one thing but there is massively different tools that we use to do those things. The challenge with the medical hypotheses trunk and and some of those other locations is um when you use the liquid symbolic or particular symbolic things that can float free, then you run into risk of those things symbolizing to unintended locations. And in fact it can be extremely dangerous. Um however oftentimes you can take down that blood supply with more conservative embolization methods like with coils and things, which is the case that that you recall. And so here's a case where we got a great result. Um but that result came from purely approximately shutting down the blood supply rather than also deeply refusing the tur with mm bullet. And so we don't even really understand what the differences are in terms of what happens long term to the tumor in those circumstances. And there are certainly going to be tumors that if you just include that acute blood supply they may go away or the you know the blood supply made it way and they made a climate there may be others where you need more diffuse um injection and with the data that that Ben's collecting. I think we're gonna get a lot a lot more information on this and and and how it can be helpful because I think that's that's a big part of what we're gonna have to figure out. There's there's we have lots of different tools apply to a very very heterogeneous disease and figuring out exactly which combinations of which things is going to take. It's it's a pretty herculean task but I think it's pretty amazing. And the only other thought I wanted to say as as the next step is the other question becomes like when um belies the subdural. You don't expect the subdural to disappear the next day or even necessarily the next week. We're doing cryonics of girls that are minimally or not symptomatic with the expectation that the patient slowly resolves it. So it does raise the question for the patients. It's very high risk for surgery. I certainly would not recommend this for patients could undergo an appropriate surgery for a very high risk patient for surgery. Is there a role for if you get an outstanding cannibalization, giving that lesion time to see if it does regress or liquefy or go in some other direction. Yeah, we've we've discussed this and I think they're absolutely is. I mean, it's hard for me to imagine that some of these will revascularization um, because they're dead. You know what I see is dead tissue. And it would not surprise me if they would regress over time. I would love to see a an equivalent of the clip versus Coyle debate emerged for some ngoma as I think that there's a potential to there's a potential to go down a route where we learned enough about which tumors might potentially be a minimal to endovascular therapy alone. Probably not all of them. I don't think that's going to happen. But there may be a way, you know, maybe a world in which we learned that some can be treated using endovascular techniques alone and not need surgery. We should we should we should continue to push the minimally invasive approach to those tumors that have been really de vascular arised. Uh huh. Because some of these cases that some of these cases just don't bleed, particularly the large ones um, that have been deeply amble. Ized, there's just no blood loss. It's not that we're worried about quantitative blood loss. It's you worry about unable unable to see what you're doing. Um, It's the bleeding, not the blood loss actually. Um So there's no bleeding that occurs and it makes it very different operation, particularly if you're inside a large tumor. You could have a very small access and get out a lot and that one I'm sure would then regress. So if you were to core out that tumor from the inside and just let it be as an intended sub total resection, that tumor then scanned weeks later I think would be much smaller. There's a good question here in the chat from doctor saying about which is probably worth adding to your research questions is does embolization affect pathologic grading of these to us. We start to see necrosis. Um Could that potentially interfere with the staging and grading of meningioma histological? I am. I think it'd be great to have a pathologist answer that question but I don't think unlike with gliomas, I don't think that to you know, having some necrosis in the specimen um up upstages the or upgrades the from a W. H. 01 to W. H. 02. I don't think that's part of the the pathologic assessment. So I think the answer to that is no. Well that's the question that I had before which is what does the M Billy's dead part look like versus navigating to a part that's still enhances that's a that's an RB that we just need to write and file and do because we could do that on tomorrow's cases by the way. I do have in the appendix but I didn't show it. Um I have done one or two of these. Well collectively we have done one or two of these that that Doctor Hodgman is has taken for the full entrepreneurs protocol with five L. A. And san active and track topography and so on. And they're just beautiful sets of images for those cases. And some of the intra may uh go a few steps towards answering dr patterson. One of the questions you asked, which is, you know, what happens using a different adjunct like fluorescents? What happens to the, you know, to the parts of the tumor that stopped enhancing with contrast? Great. And there's an additional question here about Peter, can I just say one thing real quick. I think that the question about the pathology um highlights an important thing that we really should be engaging with pathology on this and and and digging in on that exact analysis that there's probably important pieces of information that we could be getting there. Just something to think about if I can if I can make, Sorry, one more comment about that too. You know, so, you know, a lot of the genomics work as as you guys know, we work with pathology and and really the the even artistic chemistry diagnosis, just like glioma, just like Ben mentioned is moving away from meningioma as well. And the new grading categorization is really more of a genetic profile as well. So I don't think globalization and what we perceive as necrosis is going to upstage or change any of the pathology. We do and absolutely you know and I know Ben and I've talked about this. Working with pathology is going to be critical for this because there actually are vascular markers in the pathology that give us yet another quantifiable metric to look at vascular charity itself. So I mean really good point. An additional question here about whether effective mobilization, whether you've seen it have any impact on peri tumor edema in the in a few days. Well let's put it this way. There has we've never seen it get worse in the in this in this series. Um I can't say that we have uh seen it get substantially better. I would love to be given the opportunity to wait longer in some of these patients. Um and see uh so I can't at least in this series give a definitive answer one way or the other. I have seen it get worse. You know sometimes big tumor with a lot of compression. Um In fact we discuss jay and I sometimes discussed the timing to have and I. C. U. Bed ready and to have the O. R. Ready for the really big to us with significant compression just in case there's clinical deterioration not due to some giant change in the scan but um some sort of slightly increased pressure or Dema. Okay well you know it's a very simple study but we have to we have to just ask the question what's the difference between an embolism part of the tumor that no longer no longer enhances pathologically and one and the one that has not been immobilized and still enhances. That's a very important question that we haven't even addressed, which we can address. Alright. Absolutely good stuff. Any other comments questions? No. Wonderful. Thanks everyone. Thank you.