Brian H. Kopell, MD, a functional neurosurgeon who has pioneered the use of deep brain stimulation (DBS) to treat various movement and psychiatric disorders, presents work researching the use of connectomics during DBS procedures to target specific areas of the brain when treating obsessive-compulsive disorder (OCD) patients, creating a hyper-personalized approach to treatment.Chapters (Click to go to chapter start) History of targets in the brain for treating OCD with DBS Response rate for Mount Sinai patients treated for OCD with a specific DBS target, and the method for developing prospective personalized targeting Volume of tissue activated along the ALIC and white matter pathways Connectomic target for OCD Conclusions and Q&A/discussion
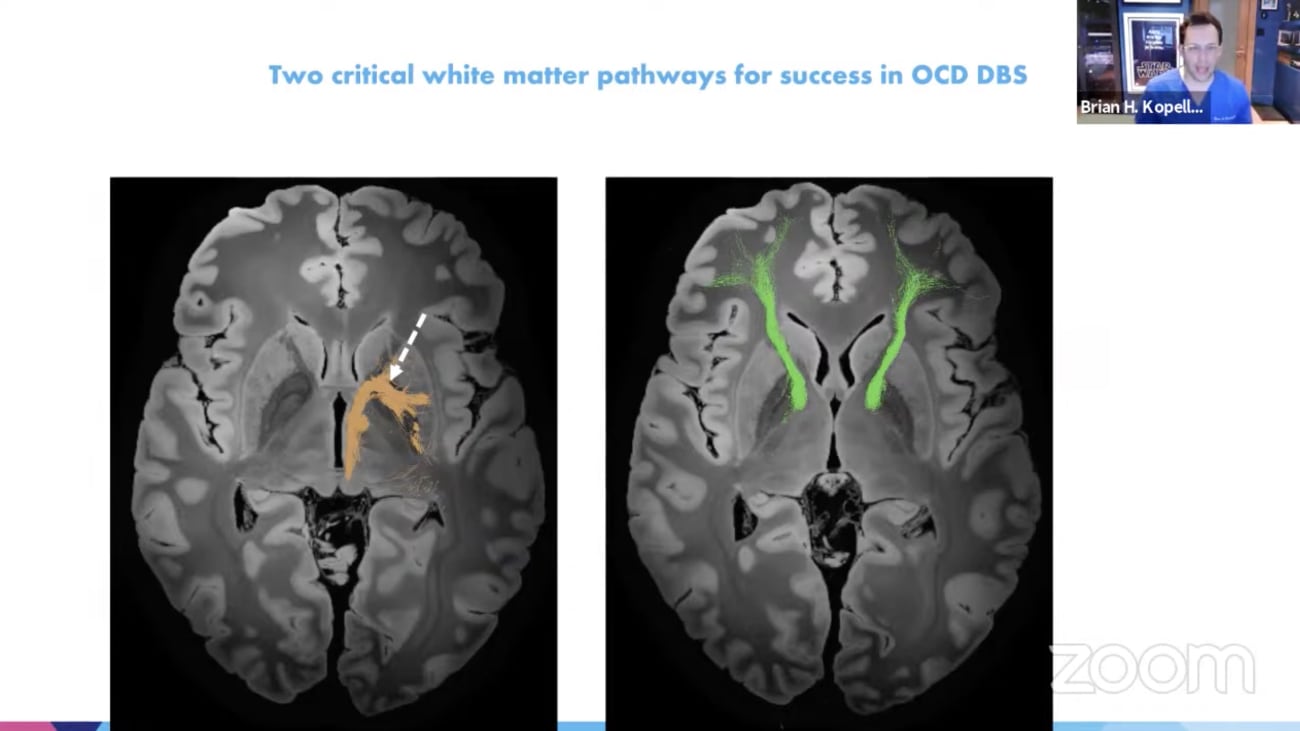
Alright there we go. And today we have got an excellent lineup. Um Here's the plan. We've got both brian couple and Tom Oxley. Hold on hearing myself in the live stream. Alright there we go. I'm sorry. Okay so we've got brian couple talking about connecting comics and DBS. Uh and then followed by Tom Oxley and being a very exciting uh set of talks here. We're starting with brian couple who is professor of neurosurgery, neurology, neuroscience and psychiatry. He's director of the Center for neuromodulation, is co director of the Bonnie and Tom Strauss Movement disorder Center. Um you can see here from his education, he has sought out additional training to become highly specialized in functional neurosurgery in standard stereotype Actiq functional neurosurgery, restorative functional neurosurgery, pain disorders. And with this training he's become a academic and clinical juggernaut and has really built a very busy burgeoning um and well respected practice. Uh that's permitted building research trials and uh and leading academics and we're going to hear today about some of the work he's been doing. Thanks very much for Uncle Bill. Thank you very much. Chris share my screen now. Great. No. So um as chris mentioned today, I'm going to talk a little bit about our group's journey towards connect atomic DBS specifically for the use of obsessive compulsive disorder since DBS has been introduced into the modern neurosurgical armamentarium in 1999. There have been a whole host of targets that have been reported used for O. C. D. D. E. B. S. Perhaps the most common is the anterior limb of the internal capsule which is itself a evolution of the capsule artemis of your. But there is a number of other targets as you can see here within the thalamus, within the nucleus accumbens region, even the habana. And you know if you look at the results of of this particular effort um They all converge about it at a 55% responders rate. And what does a responder rate mean? It means about a 35% reduction in the standard Yale Brown Obsessive compulsive scale. Now 35% doesn't sound like a tremendous amount. But this is a notoriously difficult disease to budge especially when it gets very severe. So when when you're able to move a patient that severe? 35%. That is actually really life changing um really quick primary just to give you background so that you can uh more appreciate what I'm gonna say, mechanisms of dbs. Why are fiber tracks important? So as we think about using deep brain stimulation to modulate brain and to change disease, you have to keep in mind that axons and fiber tracts are the most sensitive elements of extra cellular stimulation. So when we put these electrodes in these various areas of the brain you really have to kind of think first, what's it doing to the axons and what's the end result to the network. Um Recently there was a paper by our one of our colleagues um in in uh in Germany and in uh Amsterdam. who looked at sort of a meta analysis of all of the available uh dBS for O. C. D. Patients. And they sort of clustered where these lead placements were in a normalized brain um and overlaid a a set of track ta graffiti on that normalized brain. And what they found was essentially there were two groups responders that tended to interact with fiber tracks going to the dorsal anterior cingulate and the ventral lateral prefrontal cortex and then a more posterior group that tend to interact with fibers going down to the amygdala. But if you look at that sort of data set, it kind of implies that as long as you get anywhere along that red track which is going to go to those two critical cortical nodes, you should be able to target anywhere. Be easy, it should be an easy process to target these things. But it's not you can't just target anywhere along these tracks. There are specific areas. How do we know that well, just from experience? So one of the other sort of common themes that we have seen as a field is this interesting march posterior early from the days of capsule artemis to the days of dBS. And you can see here along that anterior limb of internal capsule, how there has been this inevitable march posterior early immediately and sometimes either door slowly eventually and we know that this is more efficient because either the patients get better or the stimulation energy needed is less indicating it's a more efficient target. But then how posterior is to posterior because once you cross that anterior commish. Sure these fiber tracks begin to diverge again fairly rapidly, some going straight to the thalamus, others going to the serotonin ergic midbrain. So in 2020 our group led by Martin, Fergie and Andrew Smith took a look at the last cohort of the patients that I've implanted um for O. C. D. And what we found in this particular cohort Um was a responder rate of 73% which is quite a bit higher than what is typically reported. Um The overall reduction in why boxes the same however, but we'd like to figure out well is this just a statistical abnormality or um is there something else behind here that we could leverage going forward for patients and so on the right hand side. Is that once again that diagram of the responders and the non responders in relation to these two tracks. And when we tended to lay our cohort onto this same sort of schema to what was interesting is that our leads tended to be in between these two cohorts for whatever reason. And so what we then said to ourselves, well aha maybe there is some sort of tangible anatomical hook that we could leverage and even further develop to make this efficacy rate. This responded rate even better. And this is a sort of an iterative process that this kind of work takes. Um The initial thing is to establish fields of volume of of of tissue activation and there are models based on gray white matter density and a given stimulation set of parameters. How much of a volume is likely to be biologically activated by a specific stimulation set. But that only gives you half the story especially when you're thinking about doing this perspectively. Uh the next thing you need to then do is take those BTS and then overlay them on patient specific white matter maps specifically fiber tracking um of the clinical response. And by merging the two you can actually begin to develop a real perspective strategy of stimulating um for these network diseases and taking this whole together this is our way of hopefully really developing an infrastructure of developing prospective personalized targeting. Yes in O. C. D. But we're doing the same and movement disorders and obviously it's the cornerstone of the work that we're doing with Helen in depression. So um this was 11 patients with treatment resistant o. c. d. that we look back on seven males for female. A meanwhile box score of 35 and the maximum score is 40. So these are incredibly sick people. And and our follow up with each patient now is four years which is quite a long period of time. So as I alluded to there's there's two types of analyses that the group did an anatomical volume of activation analysis and then looking at common white matter maps specifically tied to clinical response, not just activation but which ones did better which ones did worse than the magnitude of the effect. So the first thing was is that we had to localize the electrodes in the brain. We used a commercially available lead DBS software that that can help with this. It's open source, it's to a normalized brain. And this piece of software allows us to feed in the stimulation parameters that are being used clinically in these patients. Thus gives us the volume of tissue of activation. And we can then correlate this with the percentage of reduction in the Y box at the last follow up. So let's look at where this HVT a occurred in this patient population along the anterior limb of the internal capsule. And again we did this in an iterative fashion patient, one patient, two patient, three. We knew what their stimulation parameters are. We feed their location of their electrodes of which contacts are being used and um what that. And then we get essentially a hot spot of number of dogs cells of stimulated of of where the most likely probability of stimulus of activated um uh tissue of in these particular patients. And you can see you know the yellow area is the most probabilistic lee, high area of activation. Given the location of the stimulation electrodes and the parameters, then we can then correlate this, not just with the number of area or the area that's being stimulated. But then we can take another look at that same data set and say, well let's correlate this with how much that Y box scale went down. And in our patient cohort, the best patient had a 71% reduction in Y box. Now remember the average patient is about a 40% reduction. That's a home run, 71 is phenomenal and zen zero is obviously considered a non responder. And it was interesting to us to see how that sort of hotspot moved. Once you brought in the clinical data, the response data. And it appears that the hotspot, the areas of most activation tend to be more posterior, maybe perhaps a little bit more dorsal. And so we then said, okay, now we're we can focus in even further on that using track tomography analysis and essentially what this distilled down is the area of the highest clinical improvement, the volume of tissue that tends in a normalized brain. Now that tends to be associated with not just response, but the greatest amount of response with regards to why box reduction. And here you can see this this area at the sort of more ventral and posterior aspect of the anterior internal capsule, just above the most anterior portion of the global palace. So let's now bring in track topography into this. So This was an iterative process where we take responders. That means everybody who got at least a 35% reduction in their y box scores their responders, everybody else who got less than 35%. They are considered non responders rather than averaging them all together. Which tends to cause a lot a lot of signal dropout in the track tomography work track. Typography is especially probabilistic track. Typography is really really tough to manipulate. You can end up going down a lot of rabbit holes and um and one of the ways that we avoid this is to really just been responders separately from non responders and look at what they have, not just average but in common in terms of what fiber tracts are in fact being activated. And in um the responders and the non responding um we are seeing for instance the following. So in the non responder group there is a very unique connection that the responders don't have and it mostly involves the unscented for secularists and the amygdala feudal pathways, essentially amygdala outflow or reception to the cortex in these particular patients. For whatever reason these patients that tend to not respond, this is where their electrodes are engaging in more so than the responders conversely the responder groups have tracks that consistently interact with the dorsal A. Cc. And the dorsal medial prefrontal cortex, the ventral lateral prefrontal cortex, the anterior paladin and the sub thalamic nucleus. This is a consistent common connection that one must have to cross the threshold into being a responder and so you can really distill this back down to two critical pathways. One that I kind of alluded to at the beginning of this talk, this anterior limb fiber tract that specifically is going to the dorsal A. Cc. And the ventral lateral prefrontal cortex. And now we're beginning to see a slightly new track that's coming out this palatable thalamic tract that you can see in orange over here. Um we went a bit we went a bit further and we started to you know that's just purely looking at did you respond are you having at least a greater than 35% reduction. But then when we tried to even bend it further and look at well what about magnitude of response? What about the super responders? So here we looked at patients that had at least a 70% improvement and it is pretty clear that the amount of engagement in that frontal pathway going to the V. L. P. F. C. And the D. A. C. C. Is much much stronger than the ones that have only about a 15% response on the right okay. Um looking further down was also kind of very interesting. Um The ones that did not respond did not have that engagement in that anterior palate um going into the STN and Phil Amick regions the way that that the responders did. So there was this more posterior sort of activation of fibers tracks really focusing on that paddle thalamic area. Um putting it all together. We asked ourselves. Well maybe if response can happen if you get some of the green. Yeah you'll probably get some response and very likely you'll get some response in the orange tracks. How do we begin to merge the two in every single patient so that we can get maybe the best of both worlds. Um The critical connections of this particular frontal connection um of these of these particular cortical regions are essentially what we call the hyper direct pathway going to the anterior medial STN. Um The palette of thalamic pathway um crossing the knee of the internal capsule is on its way to to specific fill Amick nuclei, the ventral anterior and the dorsal medial uh thalamus. Um and so it occurred to us that perhaps one of the things that has driven the field more posterior lee is this in fact palatable thalamic tract that really adds to the response rate and the efficacy rate. And again, you know, putting this all together. We can sort of see where these two tracks merge and we can begin to on a personalized basis see where these tracks are in a given patient and deliberately pick a trajectory and a target point that takes advantage of that. And this is uh and this is a work that I work with kissing, our engineer on. We are now doing this in all of our patients. It's unbelievable those of you that work with with probabilistic track biography. Man, this is like working with a ham radio. Every one of these patients takes about 12 to 15 hours of just watching your computer crunch the numbers and the software that is available. It's open source and there's a great community but like the user interface is almost like a new language unto itself. It's just it's not designed to be really uh for the average clinician. Some of the parameter sets are actually the opposite of what is labeled. You have to learn to use it. And it's it's just a really hard and laborious process. But I think it's worth it. Um This is an example how we've begun to use this now, perspectively this is a recent case that we did of a patient with tardive dystonia with co morbid obsessive compulsive disorder. And so we decided to target the anterior medial STN in a way that we were able to pick up the powerful ceramic track in red and with enough stimulation pick up the yellow fibers which are those fibers going to the V. L. P. F. C. And the dorsal A. Cc. And it's still early on the kicks or so far um somewhat modulated. But what was interesting is that the IOC phenomenology has really responded first. We will see. So just wrapping it up. I just want to kind of put it all together since it's always kind of fun to speculate a little bit about what we're doing and how we're doing it. Why is the V. L. P. F. C. And the D. A. C. C. Really important in this hyper direct pathway essentially these are the areas that give us conscious control over our behavior. This is the sort of the way that we consciously engage in either uh repressing pain when we've you know we've injured ourselves and we still have to essentially perform on on the sports field. Um These are the areas that we engage in with meditation. Um But these are really really important things essentially to act as a conscious break on unwanted behavior. The how to fill Amick track. Especially the one involving the associative circuits is really involved in automatic behavior. So if the other thing is dealing with the stuff that's really under our conscious control, if you had to do conscious control of everything you would do you would you be driven mad. You need obviously a system that once you learn that behavior it reinforces it continually and allows you to execute on those behaviors in an automatic sort of subconscious way. And that's kind of what the basil ganglia does. Um It allows an automatic execution of sometimes competitive motor and emotional behaviors and then yes over time with cortical input into these areas. We can further refine this. But this is sort of a reinforce er of of of behaviors that already exist. So I want You know to kind of put it together this way you know I always talk to people that are you know the residents about like what are we doing with DBS remember it's most of the time it's it's 100 or 230. Regular stimulation hurts. That's not informational in the brain. There is no neuron that naturally You know connects and and and communicates with just regular 130 Hz. That's that's that's an a informational thing. And you can think of normal brain function and the network theory normal brain function can be thought of as essentially various different mathematical states based on all of the properties of all the different interconnected areas. And you can think of a normal brain as like a nice flat plane and the behavior the normal behavior is a ball rolling on that plane. Now due to either injury are other forms of abnormal neural plasticity. That flat plane essentially forms a divot if you will it's a mathematical divot but it's still a divot and essentially that ball instead of rolling smoothly across the plain doing letting the brain do its normal function it gets stuck. And a lot of ways a lot of these circuit pathologies are just circuits stuck in a mathematical what we call a tractor state. Um That's why I always tell patients O. C. D. Is kind of like the tremor of the limbic circuitry. So it's important to understand. Again if DBS. Isn't doing something quote informational it's not like telling the brain well you know washing your hands is completely silly because you've washed it four days ago and blah blah blah blah blah. Now essentially what DBS. Is capable of doing it greater than 100 hertz. And we know this from basic biophysical experiments is it tends to d synchronize whatever neural activity that is occurring within the state. And essentially these attractor states are essentially abnormal synchrony that's that's all it can be sort of fundamentally conceived of within these key sub circuits. So if you put an electrode in into a abnormally synchronized circuit you provide some partial or complete the synchronization of that abnormal synchrony. Then whatever the that is left of the brain that is normal will in fact subsume normal activity. So if the problem is in the conscious ability to stop and switch plans. If there is an attractor state there and you d synchronize that then lo and behold now you have a greater degree of an ability to um stop these unwanted fake thoughts and actions and the same thing can be said for an automatic reinforce er Of undesired or plans or thoughts and again this really comes out in what we see with these O. C. D. Patients it's not so much like a tremor where we turn it on always and they just set up. I don't have to wash my hands anymore. In fact one of the common things is that the behavioral therapies that were before completely useless in these patients now all of a sudden are really, really helpful in these patients. And that implies that that attractor state is gone, that the conscious and automatic inhibition areas are now online and working more properly, they're no longer stuck and therefore the brain subsumes a more reasonable state. So in conclusion, um, we're beginning to really characterize two important basal ganglia circuits associated with clinical response. This hyper direct pathway from the frontal lobes down into the STN area and an associate of paddlefish Mamic area. We believe that consistent convergences of these two pathways, maybe the personalized sweet spot for patients with OCD. And this is our central testable hypothesis for our patient cohort that we are doing in 2022. That's it, thank you. And again before I go, this is it takes a village boy. Does it take a village? This this is a work that cannot simply be done by a single person. It can't be done by two people. There's so much work and so much expertise that needs to come to bear. And um as to echo josh's sentiment in the time of year gratitude boy. Every day I wake up with a tremendous amount of gratitude that I see these people day in and day out in my work life. So I'll leave it at that. Thank you very much brian. Um if anybody has any questions, raise your hand as an attendee and we'll activate it. I see a few there. Okay, go ahead. Trevor. Hi. Thanks doctor couple. That was a great talk. Um I just had a question related to the uh study that you did, where you had the three non responders and that was attributed to the amygdala feudal pathway that was being activated. Was there aberrant track ta graffiti in those patients that such that when you place the lead that they were, it was catching more of of that pathway? Or what was what was the reason that those patients were having that pathway stimulated versus the eight responders? So Trevor, you're you're you're alluding to to really good potential possibilities. Is there a white matter abnormality in some of these patients that's gonna kick them into one direction or another? We don't know yet. We are beginning to examine that very, very issue. Um the sort of the more lower hanging fruit is just, it's a measure of the, of the the targeting, the targeting. So if you target in a certain way, remember a millimeter or two in one direction or another. And especially the angular ation. You then pick up one set of fibers over the other. It's all that's all the difference. Thank you, Jeff simmering. Hey dr Copple. Thanks for the great talk. Um I have a question regarding the reduction in the disease severity, particularly my limited understanding of the Yale and Brown OCD scale Is that half of the questions are related to obsessions and the other half are related to compulsions. So I'm wondering if you guys have looked at all if there's a symmetry in the reduction to your responders in obsessions versus compulsions or if it's a 1-1 reduction. So again, another really great question because it really speaks, you know, to sort of the sort of, I will and I'm just going to use the word anachronistic way that we sort of diagnose Psychiatric disease in the year 2021. Right. Ultimately, you know, these circuit pathologies are just based on symptom lists, which is kind of like a very 19th and 20th century way of defining these diseases and each one of these symptoms. Not every single one. But it certainly begs the question, could some of these symptoms be distinct circuits? And your point is well taken. Um, these are other areas that we're going to begin to look at once. We have a little bit more um, confidence that um that this approach is going to work. But yeah, again, a really great idea there. Thank you. We've got a question from Alex cooper um Alex. Yeah, go ahead. Hey, jeremy. Hey, dr bell thanks so much for the talk. Um, I did type the question in the chat box, which was about to talk about how understanding this variability and photography activation can change your actual surgical planning and how much variability you see between some of these patients. And then just a caveat to Jeff's question, can we have we gone to the point yet where based on their clinical presentation, we can predict variability in in white track way more attract activation or are we not there yet? So let me answer the second question first. We're definitely not there yet, we're definitely not there yet. Um you know, one of the challenges because because track tog rafi analysis is so darn laborious, you know, believe it or not not a lot of groups are really doing this at volume. So, you know, the fact that we're beginning to start to do this at volume is is we're sort of on the forefront on it. And um so we'll see um you know, with regards to personal variability, there's a tremendous amount of personal variability in this particular region. So I could give you two scans where the let's say, you can see where the STN the G P I, the red nucleus is and obviously in between them are the tracks, there's quite a bit of geometric variability from patient to patient patient. So um you know, I suppose if you really had to you could develop some sort of very complex, you know, two millimeters in front of the red nucleus in addition to three millimeters lateral to the G P. I. I mean you have to come up with some really Byzantine sort of back way of of of trying to normalize that from patients. But we don't have to do that. You know. Now we can actually just see the patient specific stuff. And yes indeed if you look at like where we end up placing the lead from an A. C. P. C. Normalized coordinate point of view it really varies from patient to patient to patient. Yes it's not like You know 10 cm away but it is within that area several several mm. And and again this is a game of mm brian brian after you put a lead in. When do you settle on stimulation parameters? How long does it take you to decide that you've optimized the stimulation parameters for that particular patient's problem. And how long does that take you have now you have variable leads where you can even change that. Right. Right. So you know there's an infinite technical space if you will josh too, you know explore in this post op period. It really still comes down to the expertise of our clinical programmers are neurologists and movement are psychiatrists and psychiatry and it's a clinical it's a clinical judgment of when they think that they are essentially Um at at Steady State. Now obviously that's not good enough is it? Right? We don't want to just rely on opinion. Right? We want to come up with something more objective. This is the 21st century. So another avenue that is being led by our colleague Alison waters is to help us develop high density e e g bio signals that can help us identify steady states so that we're not just chasing our tails. And then obviously that that also could be eventually translated to a closed loop system, Right? So Unless 71%er Did they start out like the day after that 71%? Or did they kind of ramp up as the programmers optimized? There's a ramp up. So again, you know in the in psychiatric phenomenology and not surprising in the sense of like what is the associative and limbic circuitry? You know sub serving versus like the motor circuitry right? You know in some ways our you know our experience with movement disorder DBS has been a little bit of of of an unfortunate thing and let me explain to you what I mean by that because we've all been fooled, you turn on the dbs tremor just stops dead, right? So when we started to get into psychiatric dBS first the the you know the the expectation as well, why doesn't it do the same thing? Well it's because the sort of the time course of these circuits are are are not quite as um as as fast, right? You know your motor circuit is designed if somebody throws a baseball at you at 100 miles an hour that you can hit it. That's a very very short time course. generally speaking you don't want your limbic and emotional circuitry to be so dynamic in that way. You know you want there to be a certain degree of stability so that there's a certain slowness to those circuits. That's that's a normal thing. It's a good thing. So in that regards we have to remember we're really engaging your a plasticity and so there there has to be a little bit of time, patients do report some immediate effects but it's subtle, interesting. There's gotta be other questions for brian or comments from other experts. Um can I ask a question brian? I'm fascinating talk and I think the track tomography element adds a layer of sophistication to the ability to understand the process of efficacy. You mentioned that there could be some electro physiological biomarkers that begin to emerge? Um No, I guess my question is can you give me a sense of what the biomarkers might look like and how you might use them? You mentioned in a closed loop system, but are there ways that they can be used more for targeting? And then how would that differentiate from the use in a closed loop system? Okay, great. Okay. So I mentioned now, you know networks right, Networks consists of nodes which are generally the way we conceive of it are sort of gray anatomical areas either, the parts of the thalamus, parts of the cortex, uh the STN etcetera etcetera. And then the edges which are essentially the connections between those are the white matter areas. Okay fine. So one of the ways you could develop something like a biomarker of targeting is if I put an electrode here at point X and my goal is to engage and and at least demonstrate that the electricity is is hitting. If you will just from a from a from a biophysical standpoint of of cortical region A, B and C. You could you could use that as a bio signal to say. Ah Target engagement occurs right just just from a very basic in the operating room way you could basically demonstrate that given a placement and within a fiber tract region you are in fact reaching these critical nodes of the network that you believe is important to modulate the disease. Not sexy but it's extremely attainable and and and it makes sense from biophysics standpoint number one then it's the response rate. Now that's where we can really that's that obviously is a area that's important but it can be very very complicated because right now, especially in like movement disorders, people are looking at just sort of bog standard fast for a correlations between um powers in certain frequency domains And symptom relief. Like the big thing has always been the beta peak associated with Parkinson's disease. And for about 80% of the time. That's kind of true but that's kind of a weak sauce in terms of biomarker. I you're very likely going to need to have a slightly more sophisticated double correlation between not just power and frequency but also their relationships in time as well. And so that will be another area that basically I think that people will have to look into. Mhm brian. Um I recently got my head around some of the dbs work in memory sounded like there was a lateral temporal targeting for your work. Is that what you're talking about? Yeah some kind of reinforcement of memory that occurred with some band of frequency of stimulation. And what occurred to me looking at that was the deep brain stimulation work in Parkinson's has occurred from as you said this 130 hertz which is the disruption of an abnormal circuit but this memory work is somehow causing I guess it's a long term potential Haitian or some additive effect. So can you talk to us a little bit about the difference between the understanding mechanisms of how the how the stimulation whether it's additive or or you know or it's um you know jarring. Right. Right. Right okay. So um as I said to you once you get above 100 hertz. Whatever your whatever circuit you're in you tend to de synchronize and that's generally because while the axons can fire 1 to 1 for hundreds and hundreds of hurts. The axons are great. The problems are the synapses. They're the ones that poop out in a number of seconds because they just can't um they can't recycle their their their neurotransmitters quick enough. And so as a result the d synchrony occurs. Okay but now we have this whole range of lower frequency um not only in a in a regular stimulation pattern but you know then you can start to describe pattern stimulation lower than than you know so that it gets very complicated but well if you're below the 100 hertz threshold then theoretically instead of D synchronizing you could potentially be synchronizing aspects of of activity. If that synchronization is good. Well perhaps we'll be able to help people's memory. We've already known this believe it or not. What's so fascinating about functional is that there there literally is no new thing under the sun. Oh jimin has these weird papers from these conferences that you can go find where they stimulated in the thalamus. Um And patients with tremor for instance and we know that the tremor is about 4 to 6 hertz. And you can do this in the operating room if you stimulated 4 to 6 hertz you can drive a tremor mad. It's just insane. Um And he was able to actually do some low frequency stimulation in other areas of the thalamus and either improve spatial memory or improve um abilities and um language tasks and then show when you go with high frequency how you can decorate meant it. So there there is this whole frequency domain that we can begin to just explore and then if you sort of infer from like the TMS literature where patterns of that stimulation. Theta burst, continuous intermittent blah blah blah blah blah. Could have a much much different reinforcing pattern. So that's where you're getting into that very deep end of the pool. But good question. I see that Doctor May Burke has her hand raised Helen. Do you have a question or comment? I just was going to make a comment. Can you hear me? Yep. Okay. I could I could go on if you don't need to see me but I can just talk in the air. Um But I don't know how to get in. I was just gonna say it was really nice some summary brian of the work you guys have done and its really extended how the whole field has to do this. And I will always want to comment that as you're in this neuropsychiatric space time there actually are fast things and slow things and different disorders really have to be dissected into the fast things and slow things and as a collaborator you know time is money for us to you guys have your time in the O. R. And you really it's really about where and the more that the track topography can help the surgeon to reliably go where and have tolerance limits on the lead whether it's directional or just the number of contacts. But if you miss it's over. You know this is why the psychiatrist spend they love it. I hate it. The goal is set it and forget it as your goal line And not bragging rights of how many hours it took you two. tuna patient. That's actually a mantra and it's absurd that you should be able to implant with confidence. And brian tells me all the time. He doesn't like the fact that it needs a committee to decide how to do the track topography. That's why the clinical trials fail. And we've actually reduced to practice with brian how to actually take our team approach to a Kind of three step localization for depression to actually get it in and reliably know from anatomy. We're in the right place. But then importantly how do you convince others? That's true because you're going to leave that. Oh are you need a biomarker of target engagement in the O. R. And we've been developing that with electrophysiology but we have a behavioral signal and yeah. Is it subtle? Yes. Is it quantifiable with general kind of scale? No it's individual to what someone's experiences when you're in this non cortical circuit. And once you have that you can reverse and measure a measurable biomarker might be face. We've tried to reconfigure the O. R. To look because out of the O. R. We can see it in music as a biomarker or blood pressure or pulse or skin conductance there heart rate. Those are all biomarkers we've also seen for depression. So translating that of these acute effects to then what you do in the lab outside there are two different parts. There's really surgical optimization and clinical optimization. They feed on each other. But actually I think we can get the surgical part done much faster than the clinical optimization and I think that's how we get it to practice in more people by concentrating first on the where with surgery than on the other. And then we can force in some ways that kind of structured rigor for anatomical constrained biomarkers of behavioral or office or whatever you want to do. And that's what martin and and Ki Sung and and Allison are all doing their exploring jayousi goo all these different ways to measure it And that's just the that's just the mantra of the whole approach I think. And functional we're trying to do in the neuropsychiatry space with brian. When are we going to have M. R. I. Compatible electrodes. So you can Jack right at the at the moment would that even help? Well first of all we do josh we are now the Medtronic system in particular is fully three Tesla compatible fully three Tesco compatible. Not only in the connected state but also in the disconnected state. So you can do experiments. Um Abbott is that as the same material stuff they're going to get the same connect you know approval. Um Yeah it's it's another avenue that one could potentially use maybe in the operating room to confirm target engagement. Um you know, you know M. R. I. Has a little bit of its limitations in the sense that it doesn't have quite the temporal resolution that our electoral psychological stuff has. But again sure absolutely. You know josh and and believe me it's like so thank God we have this M. R. I. Compatibility. I mean I mean when I started it was like you had to kind of sneak in after hours. I remember Pat kelly made me go with his patients after hours to the M. R. I. Um to get to get a scan and in the morning the radiologist would call up and just lose their minds basically. So we don't have to do that under the guise of night anymore. It's it's it's actually much better. I had a quick question brian that was a great talk, really appreciated that. And Helen I think you answered one of my other questions but I think brian as you look moving forward here in the field that you're defining with your team what opportunities are there for actually redesigning the lead and kind of helping you with what you're trying to focus on that was the basis of your talk. Is there an ability to to bridge a gap with better lead design Because I know that's advanced the field and a number of other designs that have come through the years, Right? So, you know, you could you could trip the light. Fantastic thinking about the differences between what you could do and etcetera. I mean, and the truth is until we get consistent results with the approach that we have now, you know, in my mind, you know, there has to be a need that technology addresses, right? So we have directional leads which are very, very compelling in terms of what they may or may not do because the idea being that if you place an electrode in a particular fiber bundle area where they're crossing etcetera, you know, theoretically one could use the different segments to differential lee engage the different circuit circuit. Um fiber tracts and modulate the circuit in an asymmetric way and maybe have a different behavioral effect. The truth is right now is that that has not yet been proven. So if we can't really if we have to really define a need of what these electrodes are and aren't doing, you know, to to really put that money in because costs, you know, you know, unlike the spine market or even the endovascular technology market, this this DBS market has not grown manifestly in years. It's at best a 708 100 million worldwide market And that's being shared by at least three major billion dollar companies. And that is a real challenge to put real R&D. In certain areas. I mean it really really is a challenge. Um you know, sure. You know, how about a lead that doesn't break, no matter what I mean. To me, that would be a great thing. You know, or a lead that cannot get infected doesn't sound sexy, but that would be really kind of a cool thing. Um lead that had a complete M. R. Transparency, that would be kind of a cool thing. Um, but other than that, I think it's gonna take some time in this sort of iterative process for us to answer that question in a way that really makes sense. Some might feel differently, but that's kind of where I think about it. I also got a question from a ha and really awesome talk and as I'm listening to all this, I'm really hoping that in our own lifetimes were able to use tracked photography for patients with disorders of consciousness and in acute coma care. Any thoughts about how far along are we in trying to be able to do that for patients with disorders of consciousness? Ryan at Lowe's lab christian dams O'Connor. They're doing some fantastic work. But we're not anywhere close as far as I can tell to two dBS and coma recovery thoughts on that. Well, you know, to sort of perspectively do like I, I can imagine like you'd want to use that for instance, let's say, a patient gets a head injury, right? And you would like to then get a scan and look at the sort of result in damage to the white matter sort of connections of areas of quote consciousness or involving, you know, the particular activating system that's gonna take like that kind of process would take you know thousands and thousands of patients to begin to correlate that with some sort of clinical outcome. What's nice about deep brain stimulation in a way is that it's both therapeutic and investigative because patients can sort of serve as their own control. You know, you can get to some of these answers more quickly. Um You know, a better person to ask would be like Nico chef Who's been working in this for like the last 20 years and that work has gone relatively slow and I think it only is because you know, it's sort of underscores the complexity and the the slowness of that work. Um Do I think it's possible? Yeah, I do think that that is the way that we're going to begin to sort of perspectively give prognosis to patients in a lot of ways. You know, not just great white matter, these tracks are so fundamentally important to normal brain function. That and along with resting state connectivity I think should be really really um I think will be important but you know, being not in that field. Um I suspect I couldn't really speculate it time. Great, looks like Helen you have another, I was just going to make a comment if the person that was interested in the um the coma and the minimally conscious, I mean nico shift and um and the stanford group actually have a brain initiative DBS project that isn't going at those people that are you know extreme. They've actually um are now doing it in people that have actually recovered but are actually looking at that same thalamic stem to improve function. And they've done a few cases and also just if you're interested in kind of discussing it with someone Tanya novel who's my postdoc at CPAc and she's over at Mount Sinai West. She was Nico Ships graduate students. She did lots of work with Pet and M. R. And pharmacology in um and many people that didn't get dbs better in that catchment. So um you know, if you're interested in that more, she um she's a local resource and I'm sure she'd love to talk about it. She's doing the emphasis on the Depression project and she's wonderful. Mm hmm. Okay, thank you very much brian for a fantastic talk. Let's move on to our next speaker. Yeah.