Mount Sinai Health System neurointensivists Dr. Alexandra Reynolds and Dr. John Liang present updates to the educational curriculum for neurocritical care fellows at the Icahn School of Medicine at Mount Sinai. They begin with the challenges in fellowship training, followed by the additions of a comprehensive lecture series and simulation training, and the creation of a ‘survival guide.’
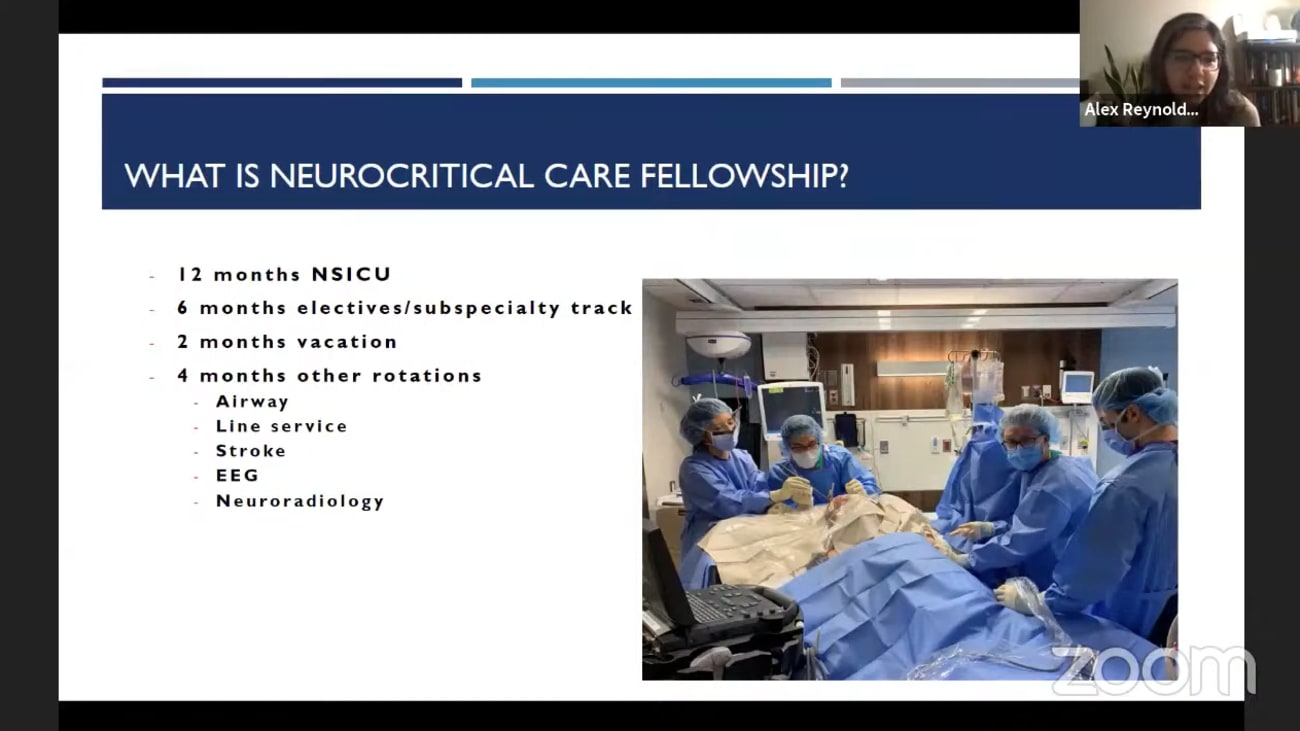
Okay, go ahead. So I have the pleasure of introducing dr Alex Reynolds, who I have known since she was a fellow and I was a resident at Cornell, She is director of the telenor critical care program and associate director of the neural critical care fellowship program in our division of your critical care. Um She completed her B. A. At Princeton, MD, A Columbia and residency and fellowships at Columbia and Columbia Cornell's combined neural critical care program and I recall are many interactions in the neuro ICU when I was a resident and she was always a pinnacle of professionalism and knowledge and continues to be um in this department and is one of my go to resources and you're a critical care on the um fortunately rare occasion that I have to take care of a critically ill adult um in this hospital. And and so I'm happy to introduce her to present to us today and then I'll pass it off to chris to introduce our next and we're also gonna be hearing from john liang who's going to co present with Alex Reynolds. John is an assistant professor of neurosurgery neurology. He's director of your a critical care at Mount Sinai West and his associate director of telling your a critical care in the Mount Sinai health system. We've worked together now for many years. I first met him when we were both fellows, me an endovascular and him in stroke. And uh we shared numerous patients with severe stroke including interested hemorrhage, large social inclusion and subarachnoid hemorrhage. He's been an exceptional ally in both clinical care and research efforts uh and also a go to person for any question related to care of these critically critically ill patients. So um now pass it on to Alex and john Let me just um share the slides. 1 2nd. Okay how's that? It looks good. Okay. Um so we were asked to speak about the division's efforts and kind of uh changing and uh updating your a critical care education within our fellowship program. So hopefully this is um not too specific to neuro critical care and um there will be some things that uh are applicable to the residents as well. So um we thought we would just kind of start with the challenges and you're a critical care fellowship training and it occurred to us that some of you may not actually know what we do or how we train. Um So we'll outline that quickly and then we'll talk about um three different changes we've made in the past couple of years. Um changes to our lecture series, um Capellas efforts, spearheading stimulation and then um the creation of a survival guide for the fellows and a PPS that rotate through our unit. Um And then john will speak a little bit about how covid has uh changed, improved and destroyed our efforts in teaching the fellows. So we'll start with what you're a critical care fellowship is um you know The basics at this hospital or that the the fellows have to do 12 months of neuro critical care. Um They have six months of electives which they can choose to direct towards a subspecialty track. Um So previous fellows have done for example six months of dedicated E. G. And then been able to sit for the E. G. Boards notably dr Riley did that when she was a fellow here. Um And then there are other rotations that are kind of mandatory in order to graduate including airway line service and then um stroke and E. G. And more recently we've wanted to do neuro radiology but unfortunately due to covid um we haven't really been able to uh get our fellows physically into those very small cramped dark rooms. Um And they haven't quite figured out how to do a remote learning for neuro radiology yet. So we're actively working on that. Um You know in terms of the fellow backgrounds I think this is one of the things that is a bit of a struggle for us within your a critical care because you can enter your a critical care from one of many kind of residency backgrounds I'd say the most commonest neurology. But we currently have fellows from emergency medicine and internal medicine and of course the famed Capital A. Was an emergency medicine doctor before becoming a neuro intensive ist. Um And then um you do have the ability to do a fellowship um unfolded through neurosurgery as well. But what that means about our trainees who are coming to us kind of, you know July one is that they all have very comfort level with various procedures. Um their ability to manage an airway and ventilate patients, um uh their use of ultrasound and then probably most importantly their understanding of neuro anatomy and the neuro exam. And so you can imagine that a neurology trained person on day one is going to be very comfortable with the coma exam and identifying herniation but may not know the first thing about intubating a patient where is the emergency medicine resident is going to be great at all the medical emergencies but may not have as much understanding of um you know, how to read a cat scan for example. And so this poses for us who are charged with teaching. Um these new fellows, it does pose a bit of um difficulty because especially if you have a class where there are people of different backgrounds, you don't really have the ability to have, like, one homogenous way of approaching education. Um I'll say that the other issue is that people come from very different hospital systems. And so there are people who have never been in a neuro ICU before who just want neuro critical care training because of their um involvement in being a consultant in a medical ICU. Uh There are people who have worked in an open neuro ICU um in various ways. And then there are people who have had, you know, four or five months of neuro ICU training already. And so even within um people who have had the same background in terms of their residency, they may not have the same comfort level or understanding of how a neuro ICU works. So that also, I'd say poses challenges in terms of how we're going to get the brand new fellows up and running. And of course it goes without saying that uh the I. C. U. Is a place where um everything is very high stakes. Um There are also a lot of demands on the fellows both in terms of their time and their attention. Um And then they're also trying to learn all the new um people that they're going to work with, including anesthesia and neurosurgery and neurology. Um And so you know, in terms of how to approach the kind of beginning of training it can be very complex. Um it also occurred to us that you may not know um what our boards are comprised of. And so I thought you know this is a busy slide but just kind of to show you that the neurological disease states are only 50% if if not a little less of our boards. And so we are mandated to understand neuro trauma, super vascular issues. Um even neurological issues such as neuromuscular disease, um seizures do violating stuff. But a good portion of our boards is actually just general medical critical care involving you know interpretation of swan numbers, understanding the next steps in assessment of acute liver failure or the next steps in um severe pancreatitis. And so we are also mandated to understand you know, concepts of general trauma um cardio, you know, differentiation of shock and advanced aerodynamics. Um And then of course within the confines of a written boards exam we only have 5% through really related to image interpretation or procedural skills. But this also goes to show that, you know, um for example if you're a neurology resident and you mostly did neurology outpatient in your residency, you may actually have a lot of issues um becoming kind of comfortable with the more advanced medical disease processes. So um you know that's the boards but then there is also the bedside procedural skills that are important. So we are expected to be able to intubate place central lines blindly or with ultrasound, bronchoscopy various imaging of the brain um at the bedside um you know, picks under floor oh Thoreau's and Perez and chest to placements. And most recently thanks to copies spearheading this. Our fellows will be learning per cutaneous tricks as well. Um And again as you can imagine an E. G. Resident who worked in a high trauma high volume trauma center may have cracked a bunch before and may not actually have a lot of issues with a tracheostomy but may not actually understand transcranial Doppler for example. And similarly uh you know neurology and neurosurgery may not be as comfortable with things like Bronx and innovations where you really need to understand the oral pharynx and the lung anatomy. So you know uh dr Setsuo and dr Riley are both um famed graduates of this fellowship program and they've had we've had a lecture series at this institution for years and years. Um And I'd say that even since I got here 2.5 years ago um it has changed quite a bit but our core electric series is twice a week um every week and you know per month we try to do um all of these things. So we do a continuous quality improvement which is our version of Q. A. Um where we try to focus on really just one case and the ins and outs of it. Um We've been doing joint Critical Care E. G. Conference um And this is a great opportunity for fellows and a PPS to understand more of the nuances of E. E. G. Reading. Led by the epileptic ologists. We obviously like the residents here we have a journal club. We have journal reviews where each um basically each participant is responsible for reading through one particular journal every day month and then just picking out the relevant abstracts and kind of um quick fire going through all the relevant papers. And this is not to be like an in depth analysis of methods but really just to kind of keep us all apprised of the relevant literature within neurology neurosurgery neuro critical Care. Um And General Critical Care because it can be pretty excessive to try to keep up with all those different journals. Um And then we have a case review. We have guest lectures either from outside the department or outside the institution. And then we do have monthly simulation now which we'll talk about in a little bit. Um And we started a research basic series. So you know the goal is to try to um have the fellows and a PPS become more comfortable with um various topics both in terms of reviewing like ancient literature that is um in your a critical care is very very few and far between. And then also kind of the most late the latest literature. Um But we do also want to be sure that they're getting enough education from outside of us as lecturers. And so you know, most recently we've had um lectures on like right right heart failure, um renal considerations in the neurological patients. So guest lecturers that can help us all, including the faculty learn about more advanced modalities from different departments and divisions that were not necessarily as comfortable with. Um But you know, actually, I believe it was dr sets use year. Um when I first came and you know, some of the residents complained, some of the fellas complained that um they didn't feel like they were all starting on the same footing. And after I've given you this kind of introduction of what you're a critical care is it probably seems obvious to you, but I'm not sure that it was obvious to us at the time um that people are coming from different institutions and different training backgrounds. And uh the thought was like, why don't we do this sort of boot camp to kind of teach everyone the basics of being a neuro critical care fellow. And so um thanks to nejad Denke Ich and her puns, we created the bolas lecture series um which was three months of intensive lectures three times a week. Um This was basically um all these lectures were divided amongst the neuro critical care attendings and the farm d that we work with. And so you can imagine from the first year that we did this, this was a huge kind of asked of all the neuro critical care attendings, because each attending was tasked with giving anywhere from 4 to 7 lectures within a three month period. And we were kind of creating a lot of these lectures from scratch because of our desire to present the material in a digestible way for people of very differing backgrounds. So these were not lectures that were given at conferences that were just recycled. These were really targeted towards um trying to um kind of level the playing field in terms of where everyone was coming from. So this is just a slide that shows the uh the breadth and depth of the lectures that we have done for the past two years for. Um are incoming fellows. And you can see on the left here it kind of ranges from the basics of neuro critical care and some of it seems very basic right? Like the exam in coma but that might be really important for an internal medicine person who has grown up used to saying um sedated cannot do neuro exam. Um There is more kind of complex pharmacological stuff like E. D. Monitoring. Um And then there's on the right there's more basic general critical care stuff. Um Airway management, ventilation, ultrasound, um arrhythmias. Um And then below that we kind of call this like being a good intensive ist understanding. Um The the topics that are really important for working in an ICU. Um but that don't necessarily um aren't necessarily just kind of factoids. And then down here is kind of how to be a good fellow, you know, how to do a proper QA how to present journal club, how to read papers properly. So um I would say that you know, we put a lot of effort into trying to do this de novo and you know, as john and I were kind of planning this bullish lecture series, we were thinking about um how we could measure whether this was what the fellows wanted and needed um as well as of course the A. P. P. S. Particularly the newer ones who hadn't been exposed to this sort of stuff before. And so um you know john has done a great job of creating uh these little google forms. And so um as uh the lecture starts, there's like a little attendance sheet that you just, there's a QR code, you just scan the QR code um and you'll see some of the data we got, we get from the attendance later. Um and then at the end we ask them to give feedback in a short survey, and I think this has really helped us understand um how to change lectures going forward to make sure that they are appropriate for the audience and you know, so for example, you know, the quality of lectures is generally very good to excellent, but sometimes depending on who the person is, um there there may already be an excellent level of knowledge at the start of the lecture. Um and so trying to understand for each topic where people are coming from and uh where we need to kind of boost them up to has been something that john and I have been trying to work on to give feedback to individual lecturers about, you know, maybe not meaning to start from the very, very basics or being able to speed through some of the, the early stuff in order to get to the meat of the lecture. Um but in general, I think we've seen that the course content seems organized and appropriate um that the information is relevant to um the neuro ICU A PPS and fellows. Um the other people who join this, our neurology residents, neurosurgery residents who are rotating in the ICU. Um and then the general critical care medicine fellows. Um And so it seems that even the critical care medicine fellows feel that most of these lectures are relevant to them, which we think is really important. So um you know, that was kind of one tier and john will talk about how later, how um that has, Our lecture series has sort of changed, thanks to Covid. Um but I did want to switch gears a little bit and talk about simulation because I think this is the other thing that in the past year has really changed about our fellowship program and I think it's been a real value. So, um, you know, we have this Star Center, it's a simulation center in the basement of uh Mount Sinai Hospital and um, it's kind of this hidden gem because there's this mannequin where you can control the pupil reactivity and size, you can make it shaken and do a kind of non convincing seizure. Um and it has the appropriate anatomy. You can hear heart sounds and breath sounds. And it's really a great option for fellows to um try and fail without harming a patient. And so, uh, cappy Lay um has been really instrumental in developing this simulation program and now expanding it to basically monthly simulations for all of our trainees and a PPS. Uh um obviously these are pre covid pictures where we could have unlimited number of people in the room, but you can see that the simulations arrange from our star neurosurgery resident abby, trying to do a very um you know, uh straightforward procedural thing to doing books, um snooze to doing um where you can see one of our CCM fellows is kind of rubbing his head and trying to figure out what the next step is. Um and so this is a bunch of uh the team trying to come up with a good plan together and we've got CCM fellow, a Palm Creek Care fellow, Alex cooper, one of our are a PPS who is very experienced and a brand new neurology resident and they're all trying to figure out the best plan for this patient. Um So you know, these are some examples of the curriculum that copy has really spearheaded so far, you know status epileptic attacks requiring the decision to intubate and the doses of medications to give. Um one of my favorites subarachnoid hemorrhage who needs an E. V. D. Um but also has a decompensating airway during the E. V. D. Placement. Um And then you know, T. B. I. With an I. C. P. Crisis where you have to kind of troubleshoot the E. V. D. On your own um patient requiring a crikey and then you know this seems kind of obvious but this is always kind of uh it seems to take the fellows by surprise. It's a catastrophic I. Ch. And really all you need to do is have a goals of care discussion with the family member at the bedside and the medical management is irrelevant. Um But you know, I'm going to see if this video plays and I hope that copies on to kind of embarrass him just a little. But you know, we'll talk a little bit about why stim is so helpful. But this is an example of an intoxicated patient who is becoming more unstable. Um And instead of just walking through the case cap is also pretending to be the mannequin. Oh john can you see if that that video works for you? Here we go. Um Kathy is pretending to be the man again. Is the sound working john. Yeah. Creamy. Yeah, but it's really meant to try to No, no, no, no, the chaos out here. I want out of here. Get me out of here! No, no, no, get me out, dad, stop, don't touch me, stop touching me. I got to take the train, Pluto Pluto. So um you know, imagine being a brand new fellow who maybe has not dealt with human dynamic instability and now has um they're attending, modifying the vital signs on the computer in the back room while being the mannequin and screaming nonsensically. And I think it it is an important thing to expose our fellows too so that they can try to kind of parallel process because obviously this is a high stress situation. Um you know, so our goal is a simulation vary depending on on the case, but I think that we all agree that there is completely an aspect of team building and understanding how to communicate with each other in a stressful situation. Review of high stakes, rapid decision making, um rehearsal of this parallel processing of of trying to figure out what to do um while waiting for help to come. And then most importantly, I think is this self reflection after the performance is done to kind of uh debrief with the fellow or the A. P. P. About what could have been done better and um you know why the patient died for example. Um So you know this now that it's become a monthly uh simulation, it's now going to require that each of the attendings do you know, plan to simulations per year, which are complex because you have to understand like um it's kind of like a choose your own adventure. You have to have plans for what to do when the um person who's doing this him makes a correct or wrong decision and you want to have very um like kind of strict guidelines for yourself about what you are going to grade. The person who's doing it on, you shouldn't just be saying at the end like, oh you did a good job or you did a bad job, but really, you know, you had the wrong joseph, the mill reknown bolas or um you know, we really wanted you to be discussing with neurosurgery, what the the target blood pressure should be or what, you know why the patient would end up going to the angio suite. So you have to have thought all of those things through. Um But we're hopeful that um this year of kind of monthly simulation will be appreciated by the fellows. Um And then the last thing that I have to give a shout out to john liang and also our senior fellow Justin grand stein who you guys have heard from before because he's done at pearls was the creation of this neuro critical care survival guide. Um I put this picture up because I wanted us to see um frank in multiple. Um but you know, this is a really important um step up for our unit where there are lots of people rotating, who may not necessarily have everything memorized or know where to go for um the important information and there is a pdf document as well that we share with um neurology residents who rotate and the CCM fellows. But um you know, this is just some examples of the work up for new onset refractory status epileptic attacks as you can tell. It's a huge checklist. Um it's not something that is easily kind of searchable on google um but it's something that when you have the patient you need to send the work up when you need to send it quickly before you institute treatment. Um you know, on the back here is doses of sedatives and paralytic for intubation. And so this was really a heroic effort by johN and Justin to really put the most high yield stuff in a book that um you know, the people who are kind of always in our neuro ICU can have in their back pocket and the rest of the rotator is can kind of have as a guide. And um Nicole from pharmacy or Farm D has been also instrumental in checking our dosages and um and I think it's just been a really valuable edition to how we have tried to um kind of streamline care for patients when there are a lot of rotate ear's who aren't kind of um consistent members of the team. So I'll hand it over to john now. Thank you. Um so you know, to pick up where Alex was talking about uh you know, I think covid has definitely um affected the way we train our fellows. It it has um had benefits and, and um drawbacks as well. So, you know, one of the things I thought was useful was to talk about it using a swat analysis and as some of you may know, a swat analysis is something that's often used in the business world, which stands for strength, weaknesses, opportunities and threats. So for the purpose of our discussion, we kind of tweaked it a little bit to think of strength as witnesses. I think the biggest benefit of the pandemic, if you can call benefit is that ah it really has helped rapidly accelerate the adoption of virtual meetings and lectures and this was really something that we were toying with pre covid since uh, we really wanted both of our, I see us at Mount Sinai Hospital in Montana West to participate in our educational conferences. However, for a variety of reasons, it never really took off until after Covid hit and we were forced to transition to virtual learning. I think we were all shocked at the dramatic increase in attendance by simply moving things to virtual. It really expanded access to our, our lectures and we now have learners from, you know, joining us from other hospitals and other departments. We do record all of our lecturers and then we can actually see that people are accessing these lectures under off time. For example, when their post call in some ways, I think um, virtual lectures has really helped with engagement uh, for some people that are less likely to speak in large group settings. You know, the ability to use a check chat function and anonymous polling is, it's definitely something that can help people ask questions and voice their concerns well having to, you know, raise their hand and speak in front of the whole crowd. One other benefit, I would say it's just the elimination of the travel time. Uh, you know, just as an example, uh, I, I used to finish rounds at Montana West and then cap it over to two M. S. H. For new conferences and I would kept back to west and That, you know, as anyone knows, Manhattan traffic in the afternoon is horrific. And so you just lose easily an hour of captain back and forth between something that's hard, a 15 minute drive or even coming to grand rounds on on Wednesday mornings and then going to west and you know, trying to make it in time for rounds. So I think having the ability to remove the travel component has really made it easier for everyone to attend meetings. You hear some of our attendance data that we actually collected um from our lecture series. So this is pre covid as you can see most of the time. The attendance is from people from outside the hospital. We do have rotator from the Brooklyn hospital. So once in a while um we have people from Brooklyn joining us and then alongside the west has been a small component most people were obviously attending live even though we try to do teleconferences, just never really caught on. Um In terms of the breakup, you know about a dirt of the um attendance was from faculty, you have fellows from neural quit and regular critical care medicine and then you have M. P. S. And P. A. S. As the bulk of it that there is, you know and the neurosurgery resident you can uh see somewhere is that there's a line somewhere there. But overall the attendance ah was quite you know, as expected for life um lecture in the unit where it's busy so people get pulled out to stabilize sick patients or post up to arrive. So our average attendance really for the lecturers pre covid was about five per lecture as opposed to post Covid, where once we moved to everything online, you know, it was actually quite dramatic. Uh We we had a larger component of people coming from outside the west and then we have people from Elmhurst Bronx, uh Larkin, you know people watching from home from Brooklyn overseas. You know actually this is um one of our current fellows Greg. So he was um in Dubai and he couldn't get a visa to come to start his fellowship in july because of Covid. So you know, despite the time zone difference, he he would actually uh log into every single one of our lecturers via zoom and join all the lectures. So he didn't miss anything when he started. So I think this is a great example of what you know uh telemedicine and tele conferences has helped us during Covid. Ah you can see the significant proportion of our attendance is now teleconference. And what's more interesting is just the people that are now joining that never joined in the past. We have stroke coordinators, we have a lot of times we have neurosurgery residency in neurology residents joining us P. A. S. And P. Epilepsy. Fellow stroke fellows, a lot of nurses, pharmacists, you know everyone is joining because it's just so easy to join. Uh and our average attendance is about 16 per lecture currently and I think that's not a unique thing. I think that's comment seen through everything that moved uh to virtual. So Elissa was actually nice enough to give me some data on, you know how our attendance for grand rounds at Mount Sinai hospital when it was live pre covid where On average we have about 55 or so attendance per week. Once we move to virtual, you know, we definitely do see an increase of at least 30 attendance per week. Um from just moving our grand rounds to virtual rounds. And who are these people that are joining? Right. Uh It's seems that it's happening to uh most of them are faculty A PPS who are normally at other Mount Sinai sites um Not my outside the hospital. So these are actually starting to attend every week rather than just coming in for the Q-8 weeks. Ah And then we obviously have a lot of no raj is no radiation neurosurgeons, Medical students from within and outside of Mount Sinai, I think the ability to eliminate the travel component is definitely a driver for getting increased attendance to our conferences. So in terms of the weaknesses or the disadvantages of covid, you know, I would say ah home distractions and financial cost is a big issue, right? Um a lot of times, uh if you have daycare issues or you have Children at home, that's home schooling, it may be a little hard for you to pay attention to conferences or log in. And there was definitely a significant rush in the initial phase where everyone was trying to buy webcams and headsets just to, they can get used to this new life. One of the harder parts of zoom based conference is really the inability to kind of read your audience, especially, you know, when the videos off you really are kind of talking to an empty screen and trying to gauge what um, whether you're connecting with anyone. Uh and while we do see a increasing attendance, I think want to unanswered questions that as educators, we still question is, you know, do you have their attention? And I'm I'm sure we have all seen or um been to zoom meetings elsewhere where someone is probably walking in the street or driving and you know, it kind of one wonders whether you do have your attention and I think that's a they struggle that everyone let's on zoom faces nowadays. Um of course, I don't have to explain to this group that there are just certain things where hands on training is hard to replicate virtually. Uh, one of my guess personal favorites is just I I. T. Issues no, um from malfunctioning audio, video, internet. And sometimes if you're really unlucky you get transformed into a cat. Uh Like this lawyer. Mr Ponton. I believe you have a filter turned on in the video settings you might want to. Uh We're trying to can you hear me judge? I can hear you. I think it's a filter. It is. I don't know how to remove it. I've got my assistant here, she's trying to but oh, I'm prepared to go forward with it. That's why I'm here live. It's not I'm not a cat. No. Right. So he is definitely not a cat. Right? Um Moving on to opportunities. So, you know, I think the pandemic has definitely presented us with many opportunities to improve our fellowship program and we definitely try to capitalize on it. Uh I think the small group simulation, you know, while we were trying to initiate it. Pre covid, I think it really took off with the need for social distancing. Where now we can take one or two people at a time, uh, into these mannequin room to get them trained as opposed to doing, um, best side training with the usual large crowd during rounds. Uh, and partly the reason why we kind of, uh, Justin and I, we really pushed to get this survival guide up and running before, um, before the new fellow started was, you know, out of fear or, you know, the uncertainty of whether with covid with with how busy we will be in the covid eunice. Do we have as much time uh, dedicated to direct teaching with the fellows? And can we impart the same uh, education as we did in previous years? So I think that really was a big driver that we wanted to get everything ready before the new fellows started. Ah turning KCC into a covid unit was really a opportunity um where our fellows were able to get exposure to non neurological pathologies that you know, which is, you know, hopefully a once in a lifetime opportunity. Um I think before covid even a home fellow cannot say that they saw 100 rds patients with multi organ failure in the span of a few months uh during the training. And so I think this is really a good opportunity for for your fellow to gain exposure to things that they would otherwise normally not see as much. And I think, you know, it's also blatantly clear that thomas and until I see you is really here to stay. So we are definitely working too, making a part of the future curriculums. I think that's a useful skill for fellow to have. Uh In addition the pandemic has probably helped um sped up adoption of other tele programs kind of like to tell the ICU program that we have and mornings I and trying to expand elsewhere, uh chris counters precision recovery program is definitely um a prime example of uh covid needs uh you know, and even tell it going back to me something that was being uh discussed and flirt around pre covid, I think maybe it might get to push the knees so something to wait for. Ah And from a institutional uh perspective, you know, these previously highly sought after physical spaces are really no longer being used and it kind of offers the institutional chance to reconsider, you know, what is the optimal usage of the space you can these be re um re allocated for? You know, maybe more, I still bet is more and more uh teaching areas, you know, something to think about and uh the research uh sorry, consent for research is another big uh improvement from the pandemic. Which you know really help make um consenting patients much much simpler for our clinical trials and Well, well there are definitely benefits and opportunities that this pandemic has offered training programs. I think we have to be mindful of these ongoing threats and challenges that we face. Uh The biggest concern probably is the risk of uh insufficient case exposure, which is a very big issue right for neurosurgeons. It usually means the cancellation of elective specialty cases for I see us. It's uh usually airway procedures like intubation and bronchoscopy which uh fellows are you know, may not get as much exposure to because we don't want them um to to be in the covid room for too long. And this is not just a no critical care. So here's a survey from the Society of Your anesthesia in their fellowship. You know, even anesthesia Trainees, only 20% of their trainees are involved in intubation is currently for COVID patients and most of the time they send the most experienced person in there so that you have a high first intubation rate and it's much quicker. Uh This actually has led to, you know, 50% of the Euro and seizure fellowship program to extend the training by about three months. Uh Certain programs who have the luxury of a research time buffer is, you know, giving up research time in order to graduate early. So, you know, the trainees are losing our research. Yeah, really, overall decreased exposure and redeployment from what your training to do to doing something that you weren't signing up for, right. Uh Same thing with american economy, a cardiology fellow, another recent survey, a majority of them had a schedule change and were asked to cover non cardiology services. A lot of them reported, you know, decrease staffing in the ecolab and uh, concern about not fulfilling the core requirement for graduation. And you have a group of cardiology fellows who are coming out reporting that they have performed fewer echoes personally than compared to their predecessors. And I think this is uh, one point that I think resonates with all of us. I think, you know, cancellations of national meetings, um, have may, you know, limit our ability to network. And um, that is something that I think we'll have to wait and see what the downstream effect of that is. Other. Other ongoing threats to consider is, you know, with everything moved to virtual, you know, we, we may lose some very well seasoned educator that just may not be very tech savvy, right? You can't really do the traditional chalk talk anymore, and it does take time to develop new materials, Alex mentioned, you know, it takes a lot of time to create uh talks from scratch and no wow facing um high end patient volumes from the pandemic. Faculty may not have damaged block time to develop new material that's uh suitable for virtual teaching. Another concern is really the erosion of camaraderie and with the free flowing of ideas that you no longer get when you're when you're not just kind of hanging out and having chit chat before and after conferences or grabbing lunch together. Uh so everyone's may not be as closing as prior budgetary constraints. As a result, Kobe is another thing that going forward, we do have to be mindful uh as to not cut funding to uh educational endeavors. You know, there are things that cost money to train, such as the same center is something that um does cost money to, to book the space. And you know, lastly, I think the most important threat that we all have to be mindful of. You know, wow is so easy to uh go from one meeting to another. You know, I think all of us may have noticed that we're getting a little zoom Fatih, we tend to just accept every um meeting so back to back and something that ah we should all be mindful of and with that, I will end with this sly of, you know, prime example of what Covid does to someone's schedule and this is NATO denktash. She uh nicely allow me to show her previous um daily schedule as opposed to her current daily schedule of what Covid does, how easy it is to get on zoom meetings, that there's just somehow more and more meetings. So uh this is I guess a prime example of a soon fatigue and with that I think ah I'll end there if we have any questions and then the other thing you forgot is that we can't hear the applause. Oh that was those three presentations were just incredible, incredible, I can't thank you enough for what you guys are doing it, even though I thought, I knew I not, I didn't know as much as I know now um you know that video you presented, Alex reminded me, I actually thought you were recording the last one on one. I had Happy, very similar For our last to our last one. Um you know this is this is really an amazing thing here, I love the idea of the book and I'm wondering if you can start to think about translating this enormous, concentrated, focused, well thought out effort into um you know, the Sinai way of doing this, but this is a comprehensive educational program. Do you have, I have not seen anything like this anywhere else, I would love to see you expand on that survival guide if you think it's appropriate. Um Yeah, absolutely, I think um it's definitely resource that um is useful for trainees everywhere. I don't think it's just useful for our unit, but it does, you know, it does include specific protocol that is, you know, quote unquote the Sinai way as you said, I think it definitely ah has an audience, How do you want to make any comments? It's taken a tremendous lift and everyone's really taken all the challenges that have come their way in their stride. So developing such a comprehensive program of course, took a massive team effort and I think Sarah Alex, john Svedala copy, everyone's really, really taken this on and are running with it in so many different directions that we didn't think neuro critical care education could have taken a shape. And I personally, not just because this is our program, but I really don't think anything like this exists anywhere else in the country or even in the world. So we are in a very unique position just being, being, uh, this amazing being, being part of this great, great department that has been very supportive of a lot of these efforts. But also we have some wonderful educators and adapting to all these technological needs, whether it's by way of simulation or using, using uh, chalk talks or zoom. I think everybody did a phenomenal job just showcasing that and converting this into something more contemporary, more uh, something that's more scalable, particularly for people who don't have access to this kind of education is going to be um, imperative, and I think we have the foundation for doing that. It's amazing. Happy. Do you want to comment on any of this? No, I mean, just to reiterate, I mean, I think people have worked really hard to to uh improve the education for the fellowship. Um, you know, for simulation, we've also expanded to critical care medicine for I C C. M, uh, and were doing, you're a critical care stimulations for the non Euro critical care fellows as well. It's a separate day entirely. Um, and I think it's given us some more visibility in the hospital uh, across critical care. Um, you know, with simulation, I think the big and now it's mentioned it, but it's it's being able to simulate really dangerous situations, especially airway situations. And I think that's the, maybe one of the primary roles. People don't get enough crash intubation in real life. You have two years to accumulate as much as you can. Uh and this really allows people to increase the numbers and go through the real time thinking that it that it involves. Um and I would just extend an invitation, you know, if there's neurosurgical residents that are interested in doing critical care stimulation, I think we can always carve out some more time. I know that critical care as part of their boards and you do a paper test, but I think uh doing this stuff in real time is very useful. Any other comments or questions from the group, the audience. Uh you know, one thing that I would also like to explore is whether through Jillian and Alyssa and the others, you can turn some of your efforts into a CMI um externally available course, I noticed in jOHN slots that he's tracking some of the people from other institutions. Um and this really might be an opportunity for you to get yourself out onto the world stage. That's a great point out of medicine and just as an example that new york neuro trauma uh consortium that respondent of Zac's efforts, we have now also been able to get CMI for at Mount Sinai neuro trauma conference. So it's totally doable and john and Alex have already been tracking these numbers, so we will certainly look into that. Thank you. Yeah. All right, well that was a really great session, appreciate it. If there are no other questions, I guess we will close it then. Thanks for having us. Thanks