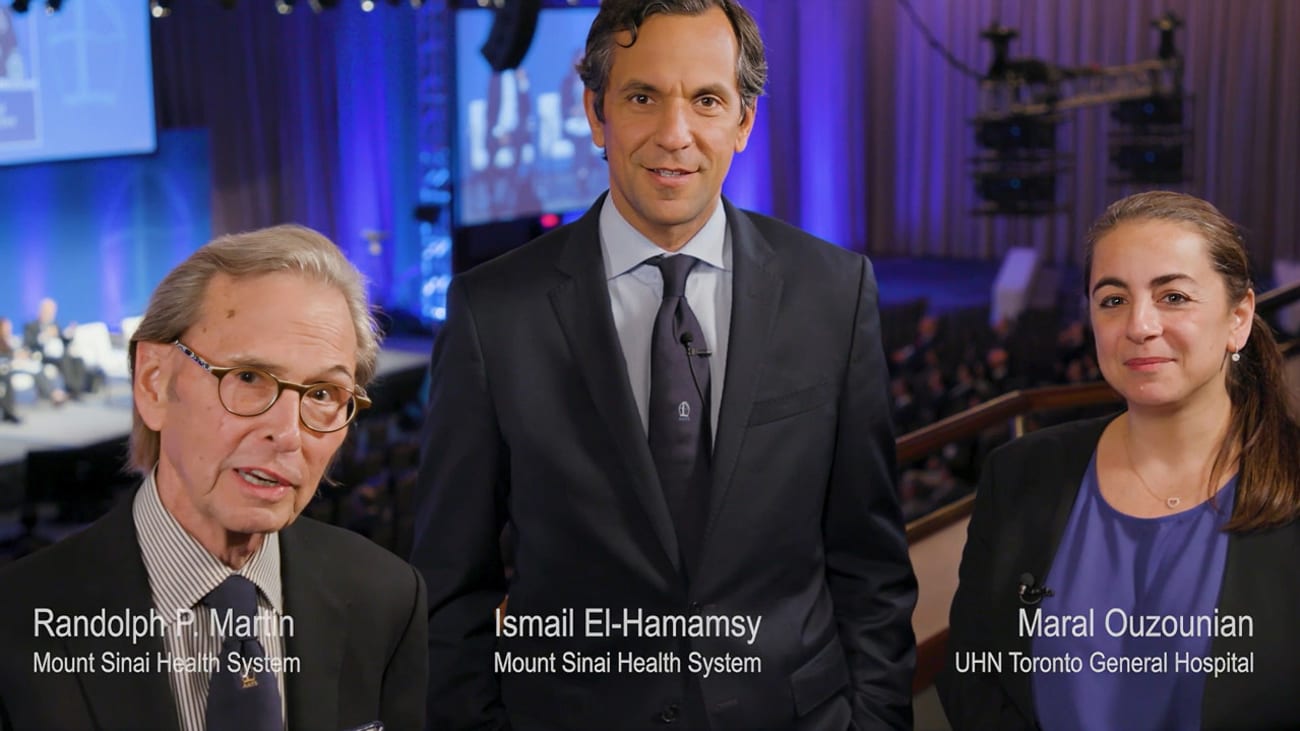
Randolph Martin, MD, speaks with Ismail El-Hamamsy, MD, and Maral Ouzounian, MD, about the lifetime management of patients with aortic stenosis and aortic insufficiency. These prominent Aortic Surgeons discuss various treatment options. They highlight that the goal of surgery is to put patients back on a normal long-term survival curve.
The doctors believe the field has evolved in a thoughtful way because there is more interaction between mitral and aortic surgeons, who work together to perform reconstructive aortic and mitral surgeries concomitantly. Dr. El-Hamamsy discusses expanding the concept of mitral valve repair reference centers to the aortic field – with multi-valve reconstruction surgeries being performed only at centers where reference mitral and aortic surgeons work together.
About the AATS Mitral Conclave: David H. Adams, MD, and Anelechi C. Anyanwu, MD, serve as the Program Directors of the AATS Mitral Conclave – a meeting that Dr. Adams created with the American Association for Thoracic Surgery in 2011. The biennial meeting brings the world’s leading experts together to examine all aspects of mitral valve disease, associated conditions, and treatment. The meeting featured more than 350 presentations, 40 focused breakout or lunch sessions, combined with four main plenary sessions – with over 900 attendees from 52 countries.
Featured:
Hi, I'm doctor Randy Martin and we are here at the 2023 A GS MIT Convoy. You can easily hear over my shoulder and I'm thrilled to be joined by two aortic superstar aortic bow surgeons and excellent surgeons. Ismael El Hazy. Good to see you man. Good to see you and me. Got to look at my script. Thank you. We had never met. So I'm thrilled I know about you and then some, thank you for joining me. We wanted to talk about aortic valve surgery. Ok, obviously, but where are we with the lifetime of a patient with aortic stenosis or aortic insufficiency? Let's say they're 50 45. Do we do ross? Do we do repair? What do we do replacement? I think what we're learning right now in aortic valve surgery is that the life expectancy and the quality of life of the patient really depends on whether or not we can offer them reconstructive aortic valve surgery. And so if the valve is repairable, that is plan C, that's the first choice repair of the aortic valve. Although in patients with valves that are marginally repairable by cuspid valves that are very asymmetrical. And where we think the repair durability may be compromised or the valve is clearly not repairable in aortic stenosis, for example, in a calcified valve, then ross would be the choice for patients who have life expectancy that warrants an operation that is reconstructive. Yeah. So what we've learned Randy is that the use of biological or mechanical prosthesis in in these younger individuals, anybody under the age of 65 or so is associated in the long term with excess mortality versus the age and sex general population. And that's all data that came out only in the last 10 to 15 years where we've been attuned to what is happening in the long term to these patients. You know, I think the focus over the last 30 40 years was how can we do safe operations and get the patients out? Nowadays, surgery is so safe that the question has become, how do we make them live a life expectancy that is normal and a quality of life that is as good as possible. And the reality is, which was rather sobering for us as aortic surgeons. When we look at our outcomes for isolated elective prosthetic aortic valve replacement in that patient population of patients under 65. That the reality is that survival is not quite the same as it should be. And so that's where the whole interest in reconstructive surgery, things like aortic valve repair or the ROSS procedure has emerged over the last 10 to 15 years and has really become the topic of interest of dedicated aortic surgeons like morale tough because that's the only way just like with mit valve repair that we can put the patients back on a normal survival term in the long term. It's interesting that the a or top of these that go along with a lot of aortic bowel disease really influence, I mean, do they, or do they not for repair? In other words? And then that's why you, if you've got to do something to the root, are you gonna do that with a repair? Are you gonna? Absolutely, I think that's uh sort of where uh the initial valve sparing operation started with isolated root aneurysms without actually a lot of aortic valve pathology, trileaflet normally functioning valve was the same principles. And if you have aortopathy and either with it by custody oric valve or leaflet aortic valve, then a valve sparing operation with reconstruction of the root and potentially leaflet repair. On top of that is the preferred option. In fact, let me add to this. We were just in a session right now. That was an aortic root reconstructive surgery in combination with microvalve repair. So a lot of these patients will come with a root aneurysm of some degree of aortic regur station. But a lot of those have also have Bar Marvin, they have Barlow mits. And so for the longest time, you would focus a lot of attention on repairing the mit and then just a little bent on, on the aortic side, or the aortic surgeon will come to a beautiful valve bearing operation and just put a, an stitch, which really doesn't last very long. It makes a lot of valves and the field now has evolved in a much more thoughtful and specific way. And that's why we as aortic surgeons are here at the Mitr Conclave is because there's a lot more interaction between aortic and Mitr surgeons around the patient so that the patient really gets the best of both worlds in terms of reconstructive A and reconstructed MIT service and you do them absolutely. But that's for a center where you've got, you, you both are outstanding aortic surgeons, but you gotta have an outstanding MIT surge there too. It's not for every place where somebody does, you know, does a few aortic or a few modules, you really need a, 100%. And that's where the the concept of centers or reference centers comes into play. I think for the in the world again, mit repair is about 2030 years ahead of where we should be. So the concept of micro reference centers, it has really become now an accepted notion and something that can be objectively measured through volume and outcomes and safety. We need to do the same thing on the side and patients who have combined disease or who have connective tissues orders who have some more of these, these conditions that require reconstructive expertise on both sides should really be funneled to centers of excellent. Absolutely. These are not that common that that's correct. And they're young patients who really would benefit in a younger patient. It matters a lot. And so it does require dedicated expertise on both the aortic, off side and on the off side. So they really should be done in centers that can offer. So let me, let me ask you two other things because I could ask you a lot, the Ross procedure because I did echoes on a lot of a lot of not so good Ross procedures in years gone by due to both of your expertise is has a resurgence going. Is it the operation of choice for patients with aortic disease? And and I believe that black who are a certain age or in certain conditions? Now, I would say so yes. And I think what the way we're doing it today is using all the lessons learned from the Ross 1.0 experience in North America, which was every center, every surgeon doing it at low volumes. And we now know that this is associated with poor safety and poor durability of the operation. So we are now concentrating these operations and centers of excellence where there's more than just an aortic surgeon. There's a whole team around the patient of dedicated cardiac anesthesia, IC U perfusion nursing that really allows for these patients to have excellent outcomes. The volumes of rosses across North America have increased five fold over the last three years and the majority of these cases are performed in large volume reference centers. So I think it's a case of fool me once, fool me twice. Hopefully, in this case, we won't be fooled the second time, right? You learn about the pulmonary side of the of the ross because I used to see a lot of the problems. I think a lot of the principles around technical details around the ross that prevent the late failures. This is what we've learned over the last few decades. And so as this mail said, it's avoiding making the same mistakes as the first time around where and if you look at the papers where the outcomes were poor, the mean volume per searcher was very low, you know, less than a few over a 20 year period. I mean, it's shockingly low and so we should not repeat that mistake. And so you really need dedicated focus and attention to actually wanting to offer Ross and not do it only a handful of times a year. I agree wholeheartedly. I'm, I'm a big fanatic on, go go to a place where the experts are or what you need done. Last question, does it sound, may sound strange? Does the directionality of the A I jet tell you about the pathology? I think it does and what you shouldn't do it. Is that well recognized? 100%? The answer is yes. And it is increasingly recognized for us who do this every day. We recognize it immediately. You see the echo, you know where the lesion is the uh but there's a lot of educating to do both on the surgical as well as on the side, as I said. And that's the reason we learn tons when we come to a meeting like this one, because microvalve repair is so far ahead of where we should be, but we can be where microvalve repair is in 10, 20 years could mean fest prolapse, non infection, correct. And the mechanisms are exactly the same. It's annular dili leaflet prolapse typically correct the prolapse, correct the annular dili. It's really the same principle actually as in my repair. But our echocardiographer are just sort of coming just waking up and so measuring the ural angle seeing how long the fused cusp is in it by cuspid valve, for example. And you know, get those things are very important clues for us to know whether or not the valve will be easily repairable or will require some advanced maneuvers. Your brain had a fabulous echocardiography very well. So, and, and they were miles ahead of the way that they were approaching. So I think that's great. Well, I'm, I'm encouraged that uh that, that, that uh you know, excellent aortic surgery is, is close at hand for us. For all of us. So thank you both. Thanks. Thank you. Good to see you in person. Thank you and thank you for joining. Thank you.